When a $0 reimbursement is posted to a Second Review submission, daisyBill automatically moves the Bill to Processed status, generates a Denial EOR - Second Review task and assigns the task to a designated daisyBiller.
To complete the Denial EOR - Second Review task determine whether additional funds remain due for the bill.
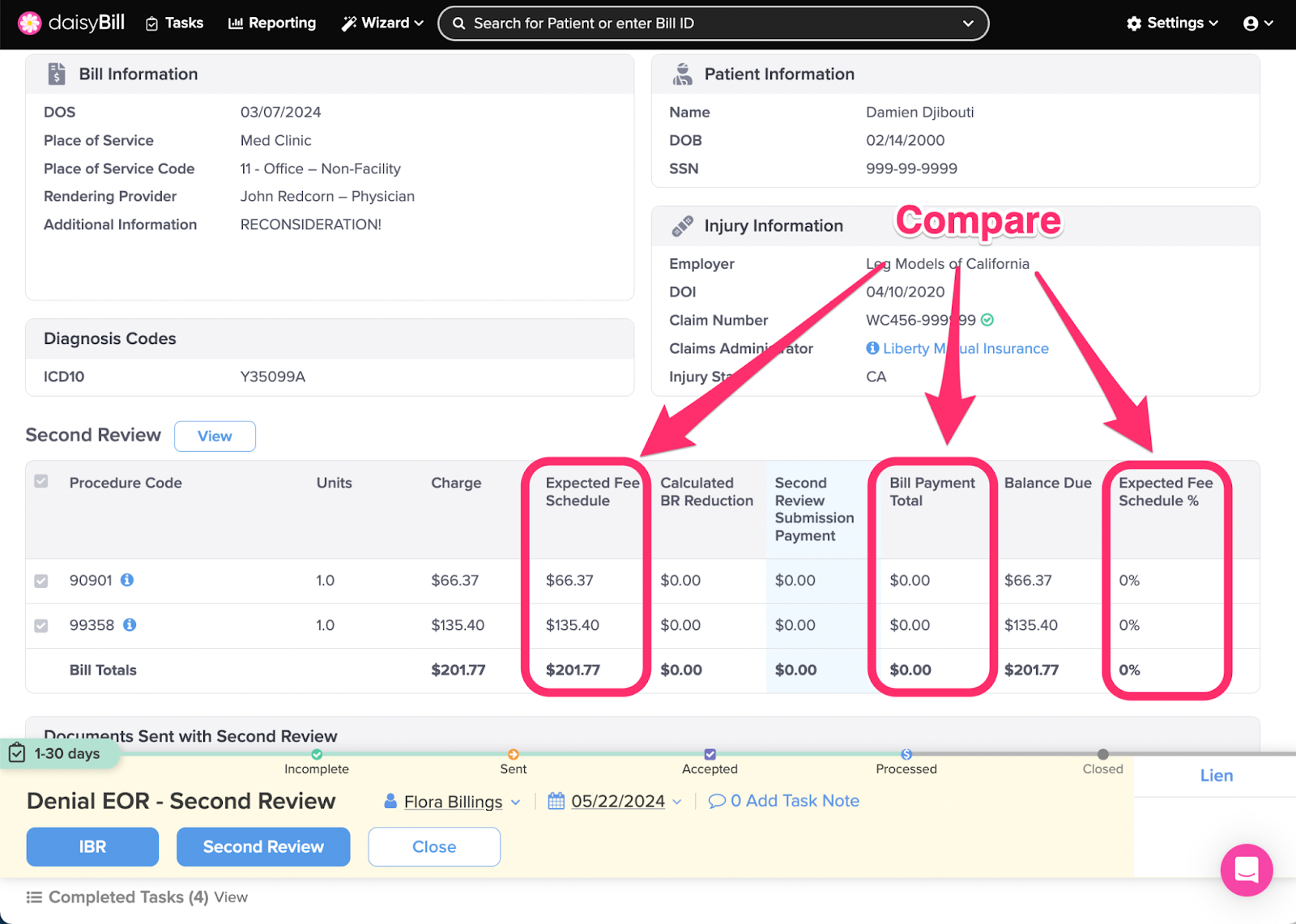
Step 1. For each Procedure Code compare the ‘Expected Fee Schedule’ amount to the ‘Bill Payment Total’
Expected Fee Schedule: daisyBill calculation of state fee schedule (for supported states), or, Organization's set Expected Reimbursement.
Bill Payment Total: Total of all payments posted to all submissions of the bill.
Expected Fee Schedule %: Bill Payment Total divided by Expected Fee Schedule.
Balance Due: Expected Fee Schedule less Bill Payment Total.
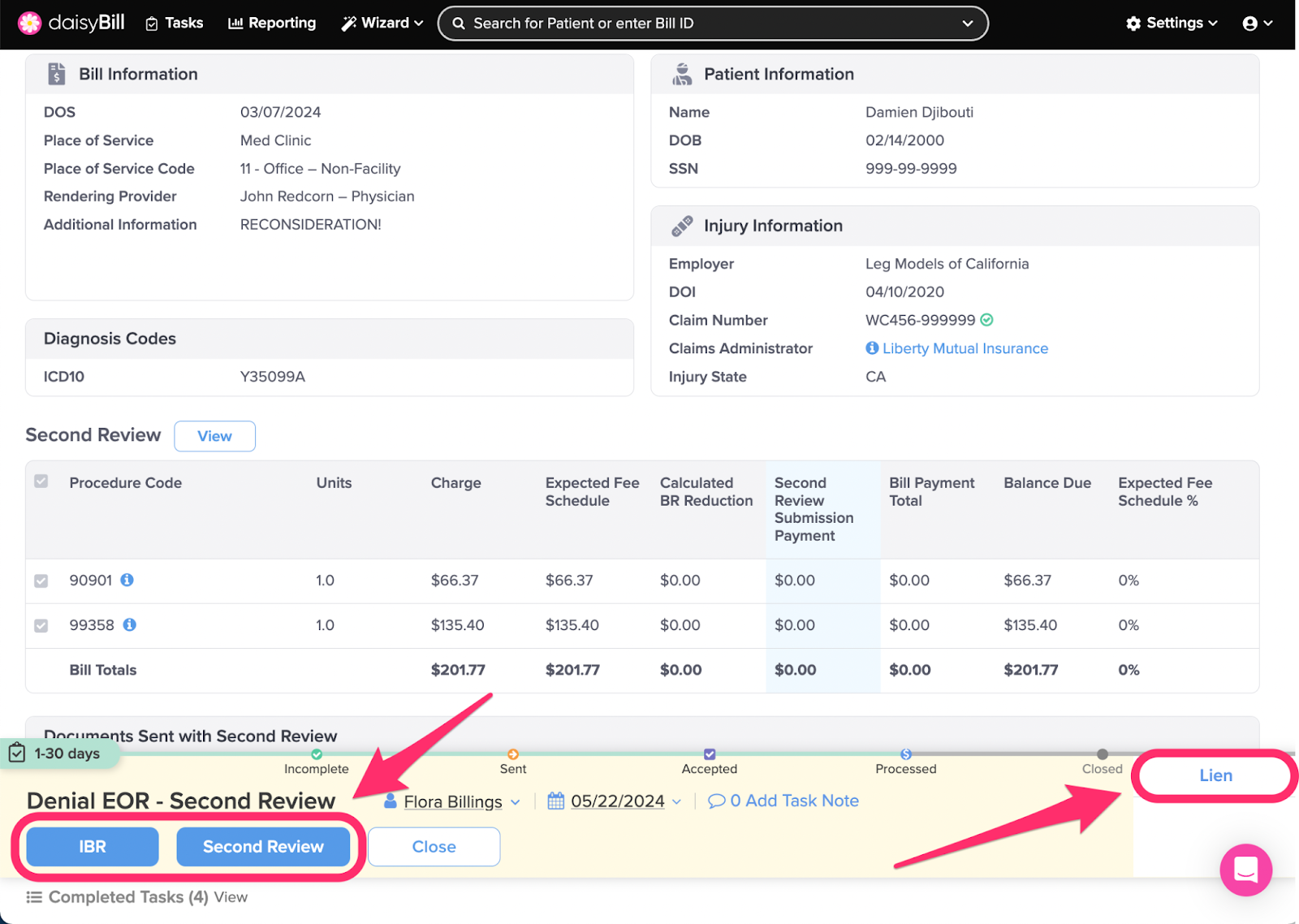
Step 2. For insufficient payments, choose an option from the ‘Action Bar’
IBR: Changes Bill Status to Incomplete, navigates to the Independent Bill Review (IBR) function to create an IBR submission. For more, see the Help Article: Create IBR Submission.
Second Review: Changes Bill Status to Incomplete, navigates to the Second Bill Review (SBR) function to create an additional SBR submission. Claims Administrators are only required to process one Second Review.
Lien: Changes Bill Status to Lien, queues the bill with all other bills for the injury marked for Lien status. (But does not file a lien. This must be done outside daisyBill.) For more information, see the Help Article: Mark Bill as Lien - Lien Filed.
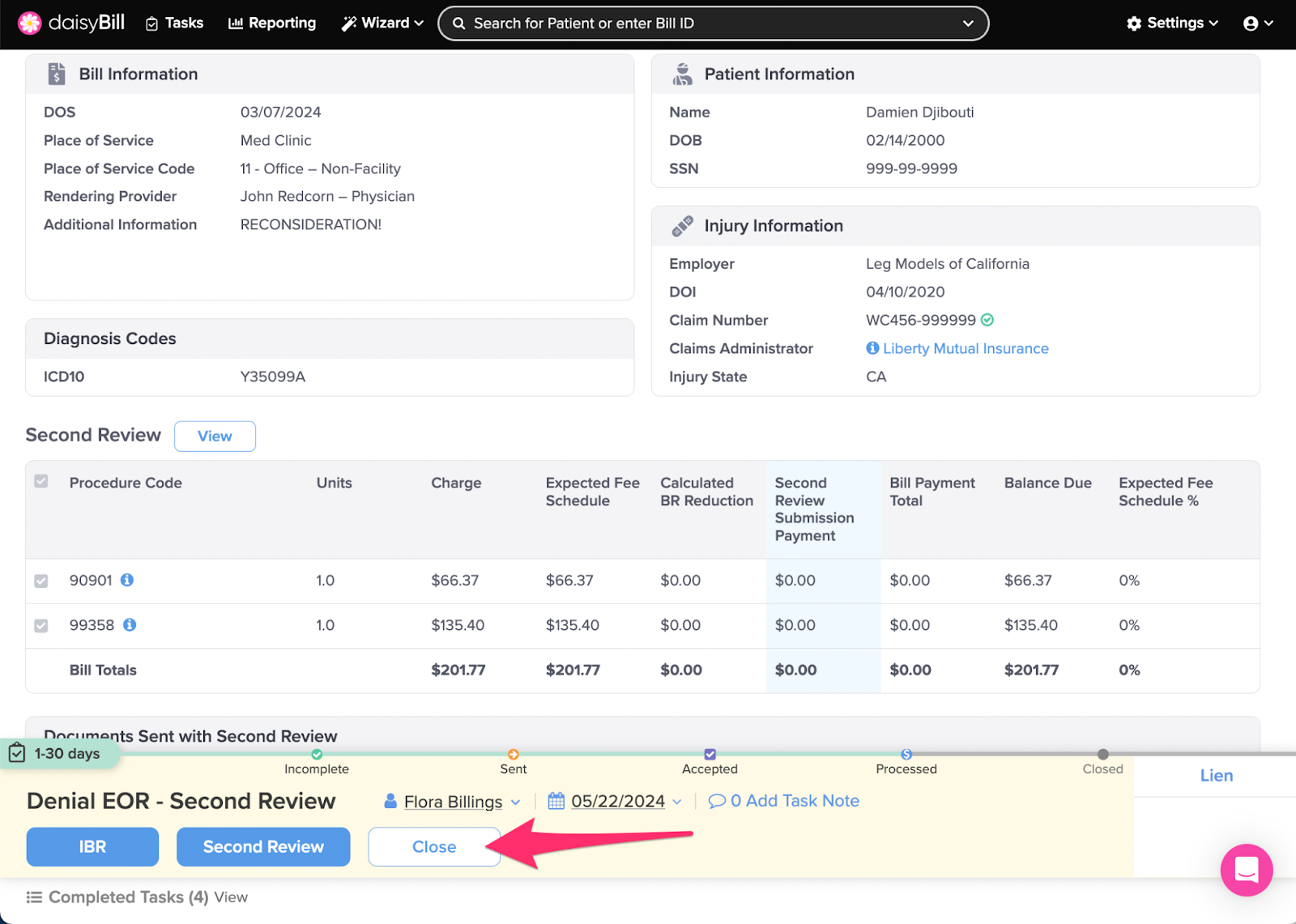
Step 3. For sufficient payments, click ‘Close’
This moves the Bill to Closed status and completes the task.
Simple!