Getting an NCCI Edit warning? Don’t worry. Here’s how to fix the error.
California regulations require reimbursements factor in these fee-affecting rules:
- Physician NCCI Edits: These National Correct Coding Initiative edits affect allowable combinations of different procedure codes.
- Practitioner Services MUE Table: These Medically Unlikely Edits affect the number of allowable units for a given procedure code
Since claims administrators may deny reimbursement for the procedure codes that violate either of these rules, daisyBill alerts you of any NCCI errors. Depending on the rule violation, correct the bill by doing one of the following:
- Adding an appropriate modifier
- Selecting a different procedure code, or
- Editing the number of reported units
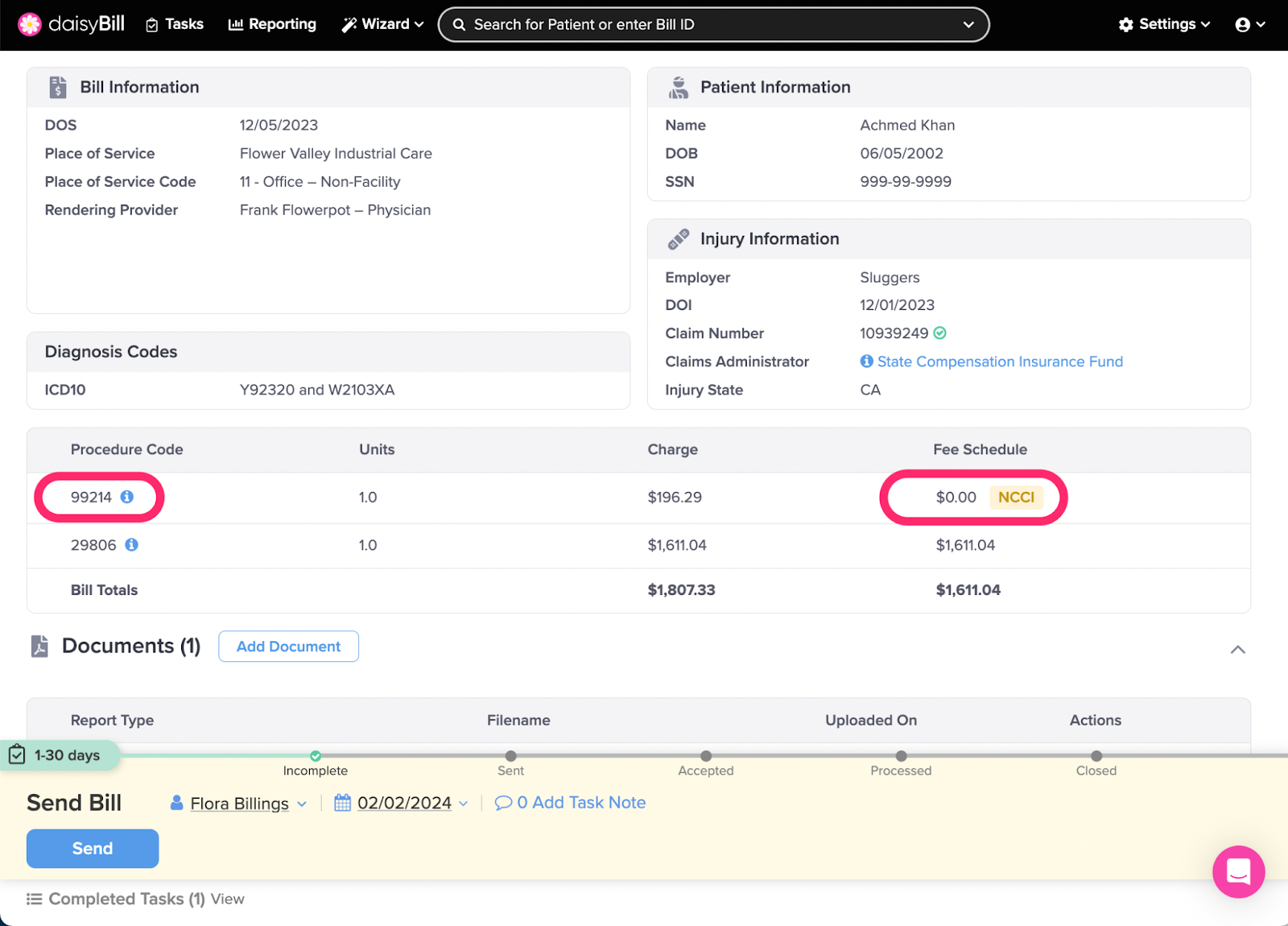
Step 1. From the Add Bill Page, enter required information and click ‘Create Bill,’ then review for an NCCI Edit warning
If the Expected column shows $0 and a yellow NCCI Edits warning appears next to the procedure code, the bill violates an NCCI edit.
Step 2. Click the ‘i’ icon next to the Procedure Code
Clicking the icon displays detailed information about the NCCI Edit or MUE error.
NCCI Edits occur when services are incorrectly billed together.
- The NCCI includes code pair edits, where each edit has a ‘column one’ and ‘column two’ HCPCS / CPT code. If a provider reports the two codes of an edit pair, the ‘column two’ code is denied, and the ‘column one’ code is eligible for payment.
MUEs prevent payment for an inappropriate number/quantity of the same service on a single day. MUEs are adjudicated either as claim line edits or DOS edits.
- If the MUE is adjudicated as a claim line edit, the units of service (UOS) on each claim line are compared to the MUE value for the HCPCS/CPT code on that claim line. If the UOS exceed the MUE value, all UOS on that claim line are denied.
- If the MUE is adjudicated as a Date Of Service (DOS) MUE, all UOS on each claim line for the same date of service for the same HCPCS/CPT code are summed, and the sum is compared to the MUE value. If the summed UOS exceed the MUE value, all UOS for the HCPCS/CPT code for that date of service are denied.
Step 3. Edit the bill and correct the coding
Step 4. Check the NCCI Edit warning
The warning turns green and displays a Fee Schedule amount when it is successfully corrected or overridden.
Step 5. Learn more about NCCI Edits: CMS National Correct Coding Initiative Policy Manual For Medicare Services
NCCI Edits cover many different correct coding topics, including:
- Misuse of column two code with column one code
- HCPCS/CPT procedure code definition
- Sequential procedure
- CPT "separate procedure" definition
- Anesthesia service included in surgical procedure
- More extensive procedure
- CPT Manual or CMS manual coding instructions
- Standards of medical / surgical practice
- Gender-specific (formerly Designation of sex) procedures
- Standard preparation / monitoring services for anesthesia
- Laboratory panel
- Mutually exclusive procedures
- MUEs
That’s a lot to digest, we know.
To sum up: daisybill shows a yellow NCCI Edit warning when it detects coding errors. When the coding is corrected, the yellow error message turns green.
Go forth and submit with confidence!