For bills with a No Response Task, you may choose to call the claims administrator to obtain the bill status.
To help you record the outcome of your call, daisyBill provides five possible Bill Payment Status options.
- Message Left Requesting Bill Payment Status
- Explanation of Review / Benefits (EOR / EOB) Pending
- Explanation of Review / Benefits (EOR / EOB) Sent
- Bill Not on File
- Bill Forwarded to Different Payer
Each option prompts you to report key information from your call with the claims administrator.
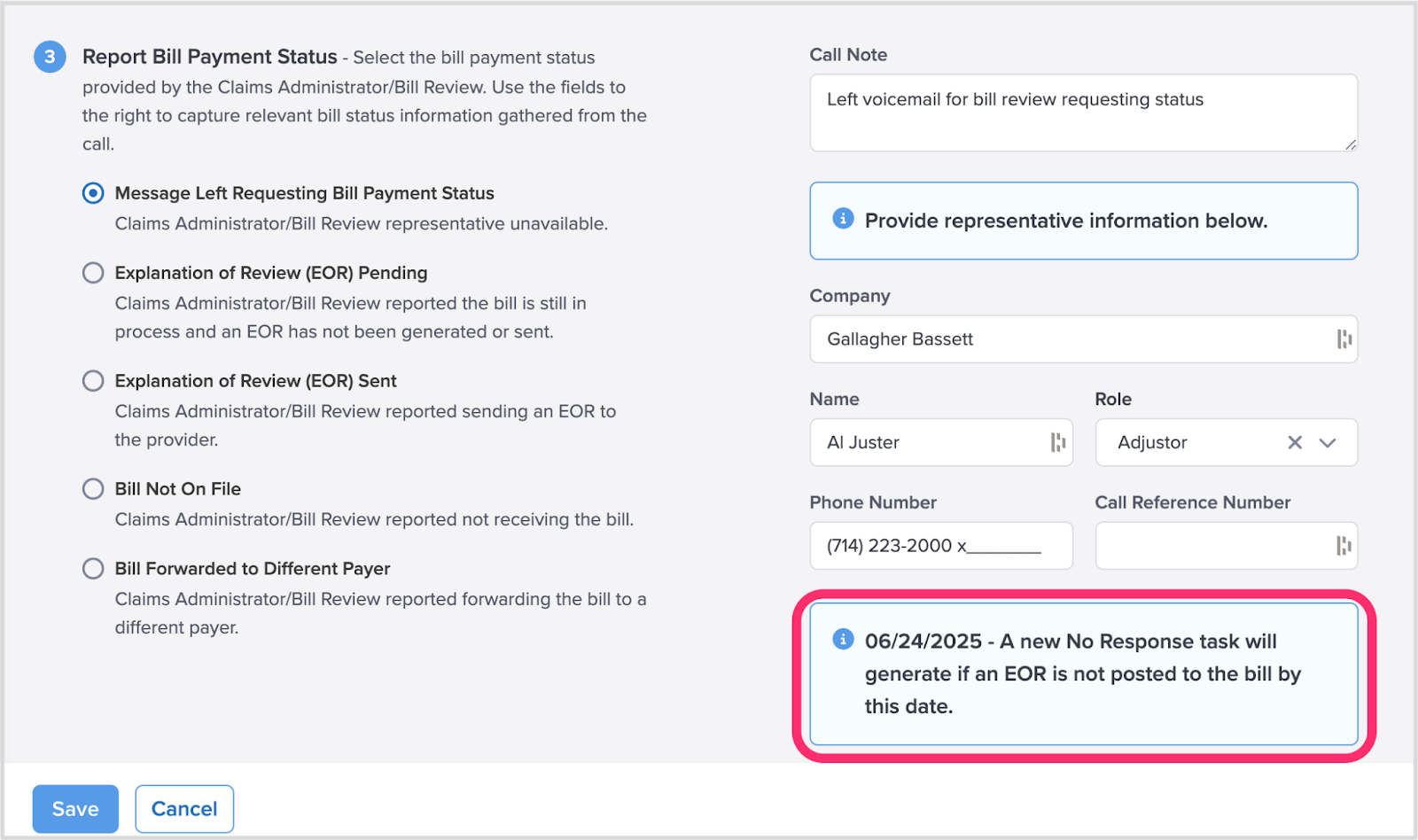
Option 1. Message Left Requesting Bill Payment Status
If the Claims Administrator is unavailable, select ‘Message Left Requesting Bill Payment Status’ and enter the claims administrator representative's information.
If an Explanation of Review (or EOR) is not posted to the bill within 5 calendar days, daisyBill automatically generates a new No Response task for the bill.
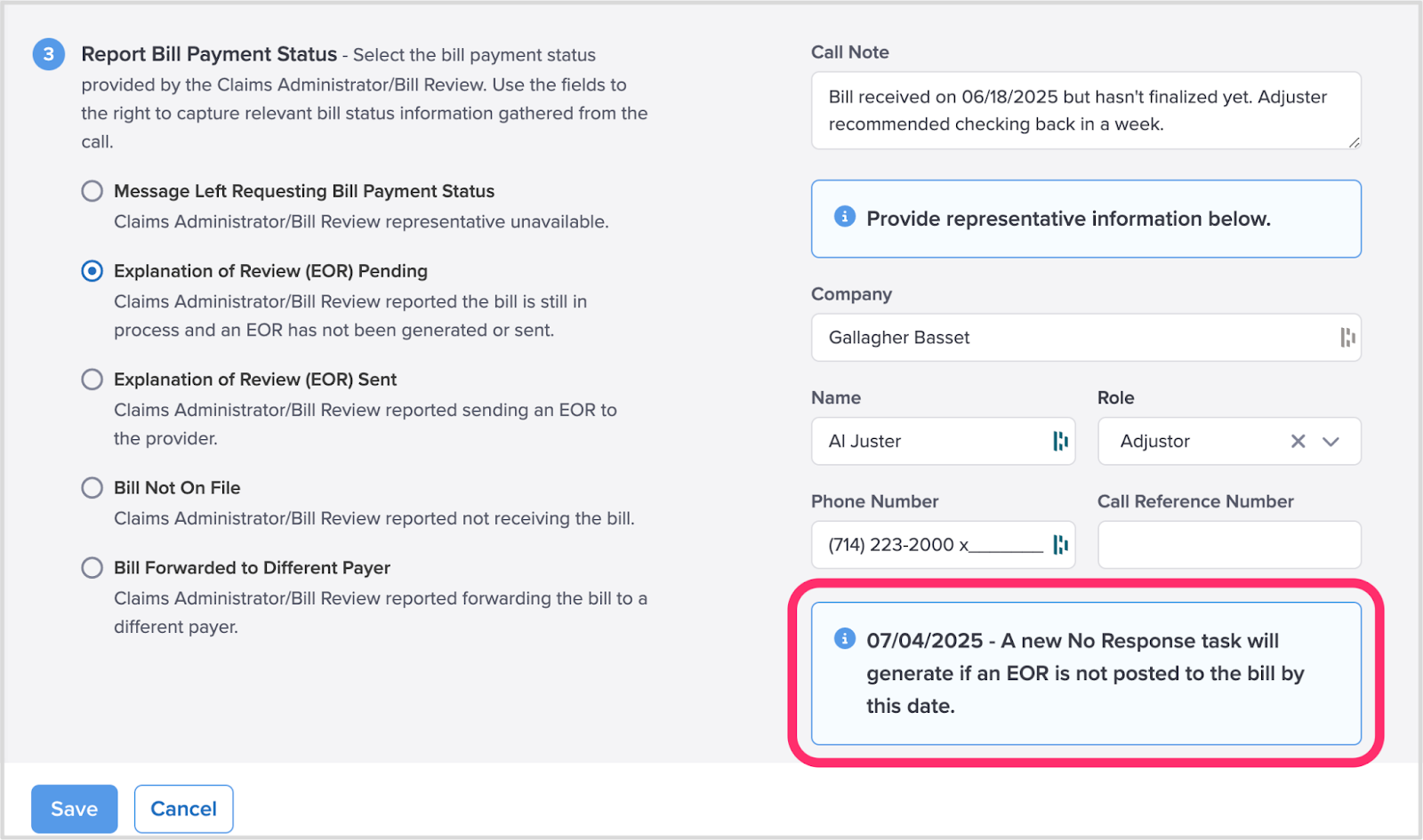
Option 2. Explanation of Review / Benefits (EOR / EOB) Pending
If the claims administrator representative acknowledges receipt of the bill but has not issued an EOR/EOB, select ‘Explanation of Review / Benefits (EOR / EOB) Pending’ and enter the claims administrator representative's information.
If an EOR/EOB isn’t posted to the bill within 15 calendar days, daisyBill automatically creates a new No Response task for your practice.
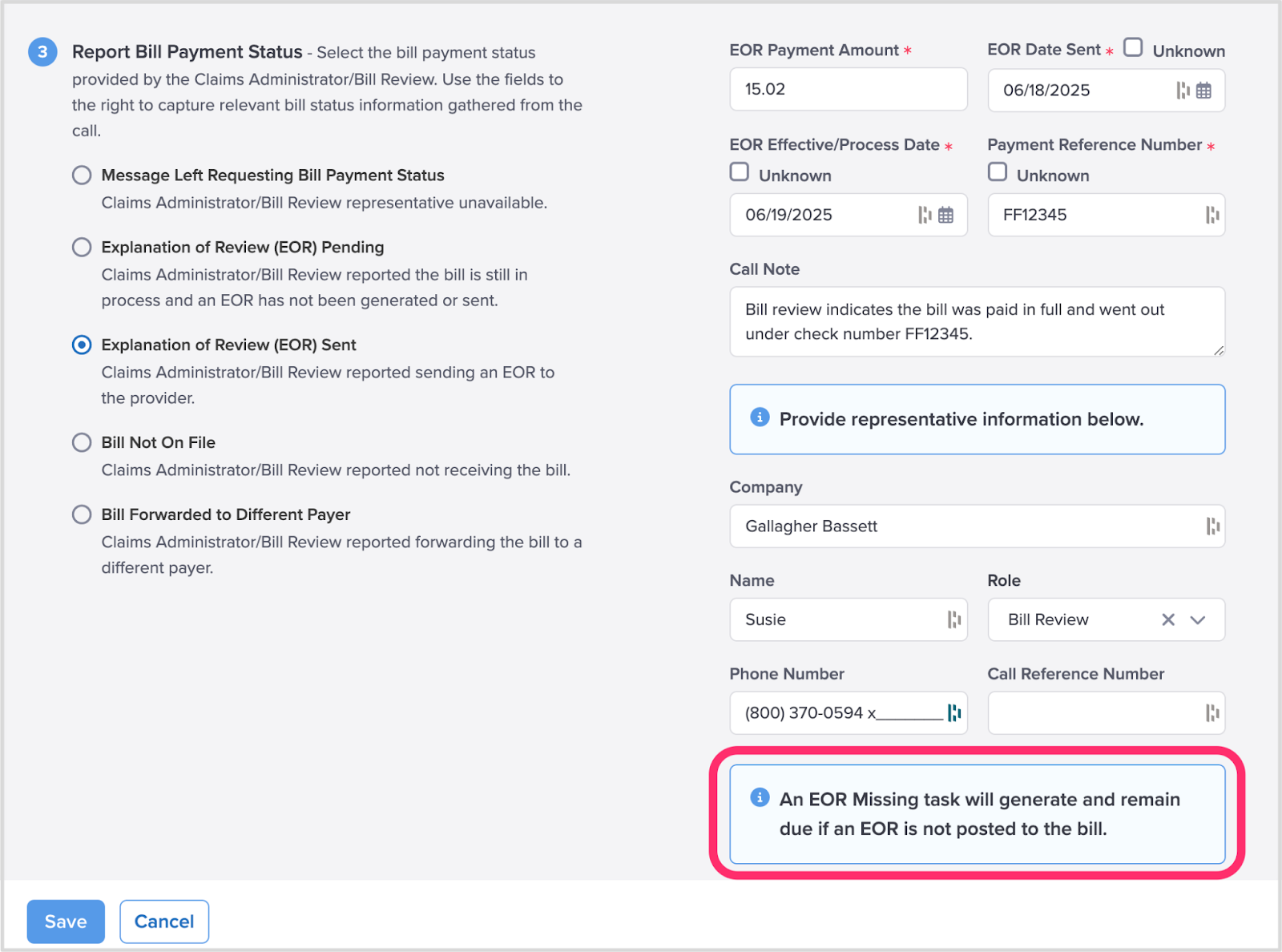
Option 3. Explanation of Review / Benefits (EOR / EOB) Sent
If the representative reports sending an EOR/EOB to the provider, select ‘Explanation of Review / Benefits EOR / EOB Sent’ and enter the payment information reported on the EOR/EOB.
daisyBill automatically generates an EOR Missing Task alerting you to locate and post the EOR/EOB payment.
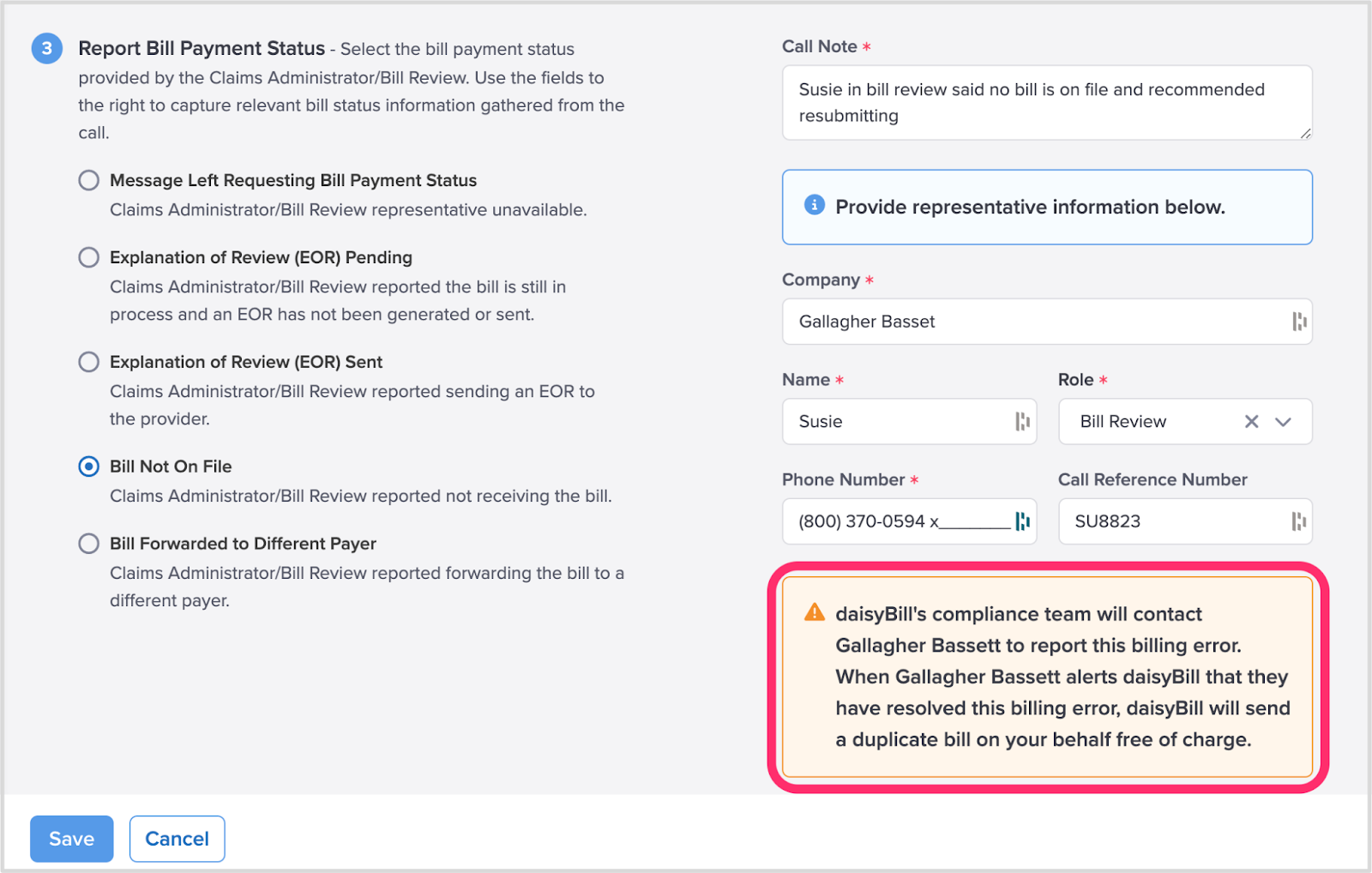
 Option 4. Bill Not On File
Option 4. Bill Not On File
If the representative reports not receiving the bill, select the ‘Bill Not On File’ and provide the claims administrator representative’s information.
The daisyBill compliance team will contact the claims administrator to report the claims administrator’s billing error.
Once the claims administrator confirms they’ve resolved the issue, daisyBill sends a duplicate bill on your behalf—free of charge.
Option 5. Bill Forwarded to Different Payer Status
If the representative reports forwarding the bill to a different payer, select ‘Bill Forwarded to Different Payer’ and enter the new payer’s information.
If the different payer doesn’t remit payment within 15 calendar days, daisyBill automatically creates a new No Response task.