When an original bill is incorrectly denied or underpaid, daisyBill advises filing a Second Review. Every request for Second Review submitted from daisyBill is compliantly submitted using both a completed DWC Form SBR-1, as well as a compliant modified CMS 1500.
To store language for Request for Second Review reasons in daisyBill, use the Second Review Reasons. When a bill receives an incorrect denial stating services were not authorized, we recommend language similar to the Second Review reason in this article.
Official Medical Fee Schedule
Any
CPT Code(s)
Any
Payable
Yes
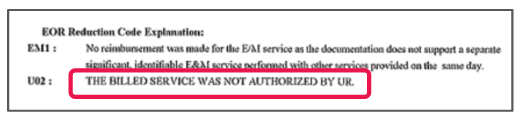
EOR Denial Reason
The billed service was not authorized by UR.
Second Review
Reason for Requesting Second Bill Review
The services billed were authorized by UR. Please immediately reprocess this bill and issue payment. Attached is the Utilization Review authorization.
[When SCIF is the claims administrator] We have been informed that SCIF automatically denies bills based on internal adjuster notations regardless of authorization status.
Please immediately reprocess this bill and issue payment.
File Second Review