When a reimbursement is posted to a Second Review, daisyBill automatically moves the Bill to Processed status, generates a Payment EOR - Second Review task and assigns the task to a designated user.
To complete the Payment EOR - Second Review task determine whether additional funds remain due for the bill.
For incorrect reimbursements, timely completion of Payment EOR - Second Review tasks guarantees timely submission of the Independent Bill Review (IBR) request within the 30-day mandated timeline.
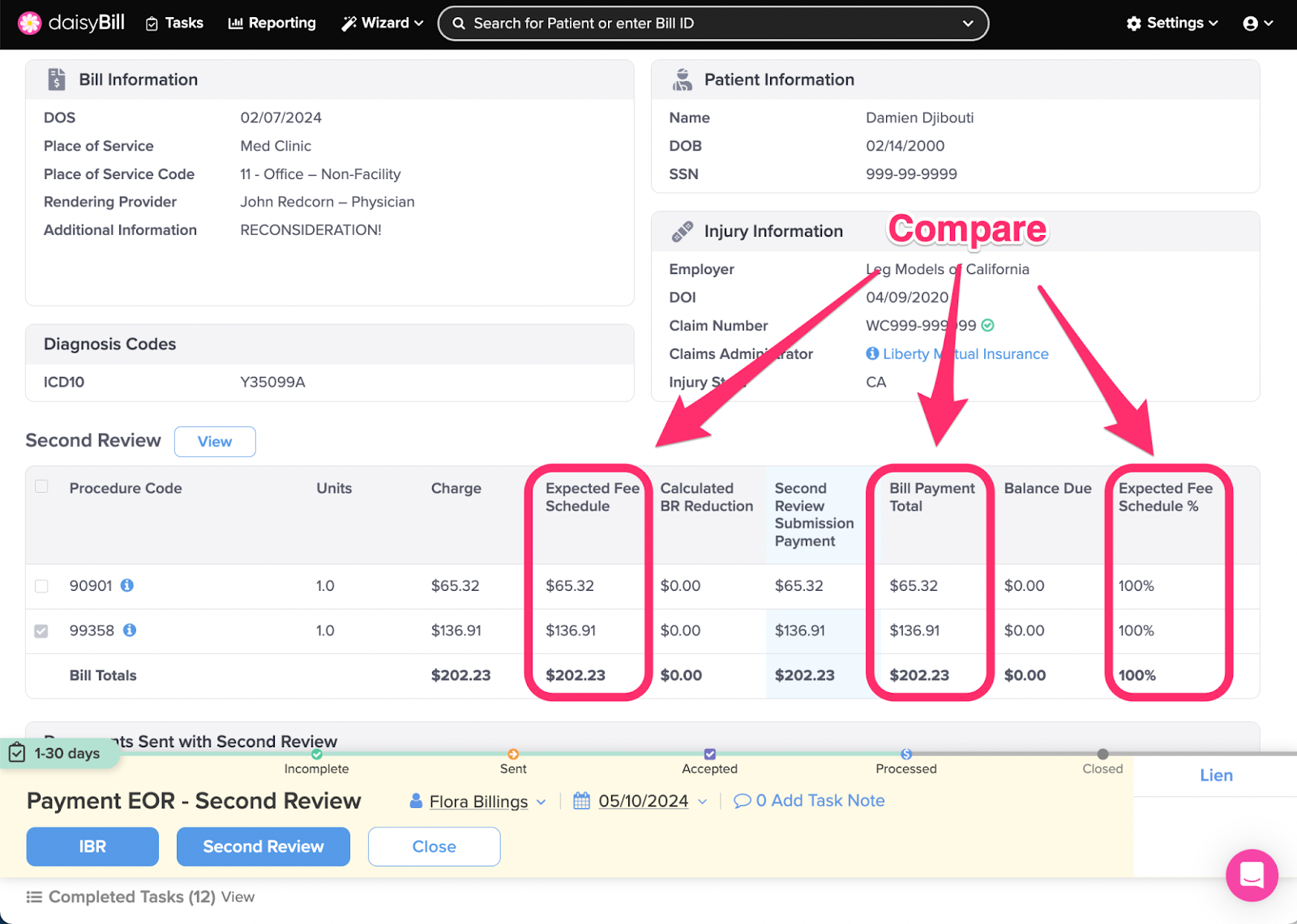
Step 1. For each Procedure Code, compare the ‘Expected Fee Schedule’ amount to the ‘Bill Payment Total’
Expected Fee Schedule: daisyBill calculation of state fee schedule (for supported states), or, Organization's set Expected Reimbursement.
Bill Payment Total: Total of all payments posted to all submissions of the bill.
Expected Fee Schedule %: Bill Payment Total divided by Expected Fee Schedule.
Balance Due: Expected Fee Schedule less Bill Payment Total.
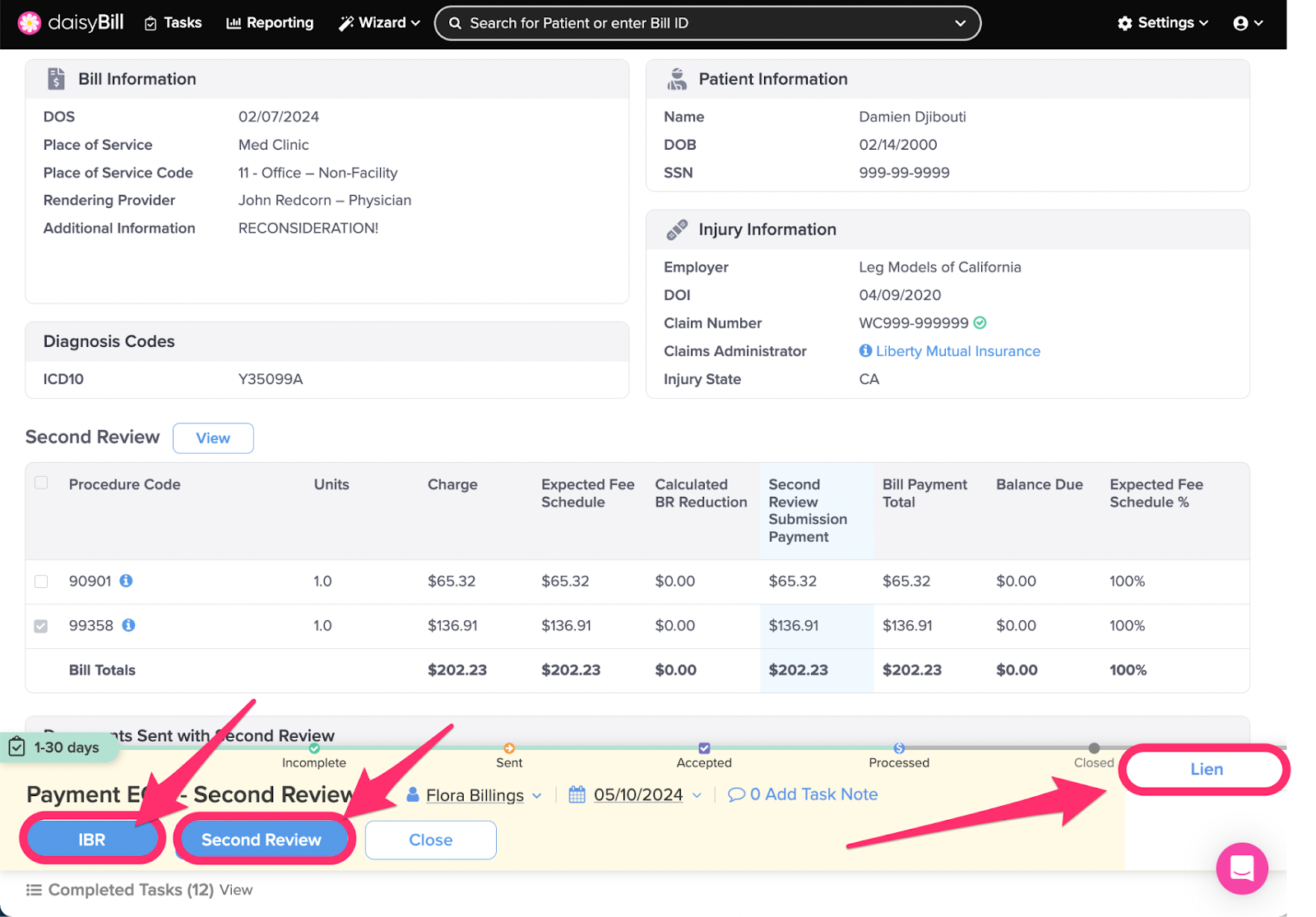
Step 2. For insufficient payments, choose an option from the ‘Action Bar’
IBR: Changes Bill Status to Incomplete, navigates to the Independent Bill Review (IBR) function to create an IBR submission. For more, see the Help Article: Create IBR Submission.
Second Review: Changes Bill Status to Incomplete, navigates to the Second Bill Review (SBR) function to create an additional SBR submission. Claims Administrators are only required to process one Second Review.
Lien: Changes Bill Status to Lien, queues the bill with all other bills for the injury marked for Lien status. (But does not file a lien. This must be done outside DaisyBill.) For more information, see the Help Article: Mark Bill as Lien - Lien Filed.
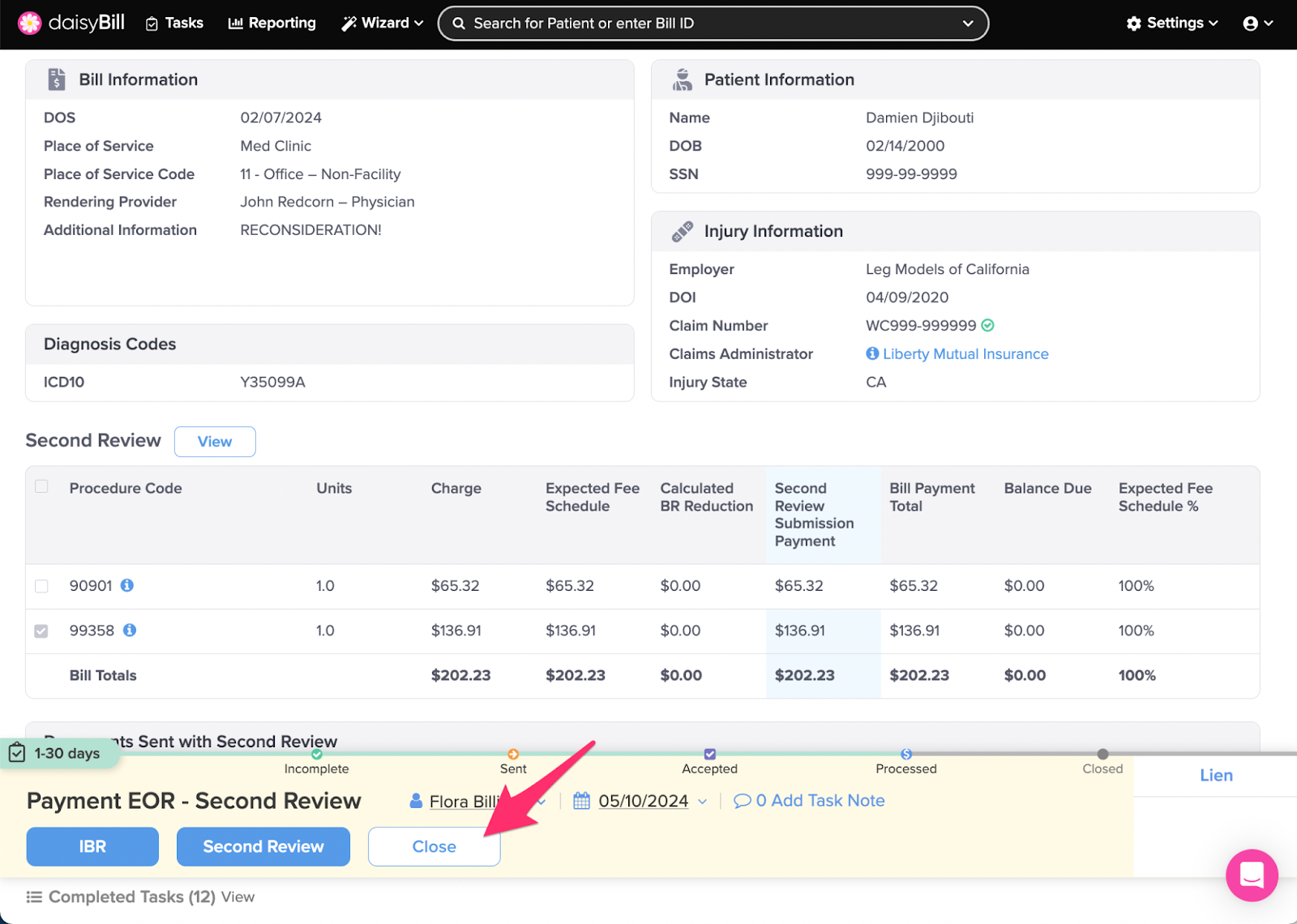
Step 3. For sufficient payments, click ‘Close’
This moves the Bill to Closed status and completes the task.
You’re all set!