Summary
Treating physicians are required to submit a complete and compliant Request for Authorization (RFA) for treatment.
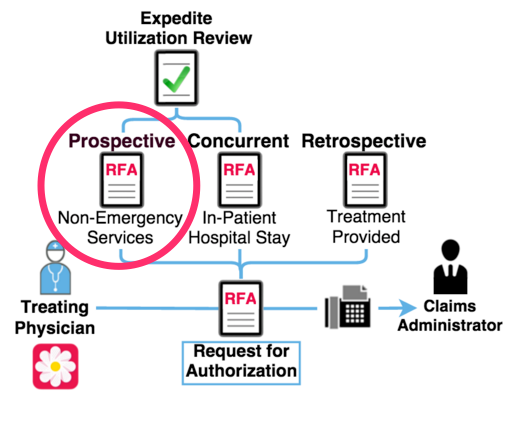
There are three RFA types: concurrent, prospective, and retrospective.
Regulation 9792.6.1 defines a prospective review as any utilization review conducted prior to the delivery of the requested medical services, with an exception of utilization review conducted during an inpatient stay,
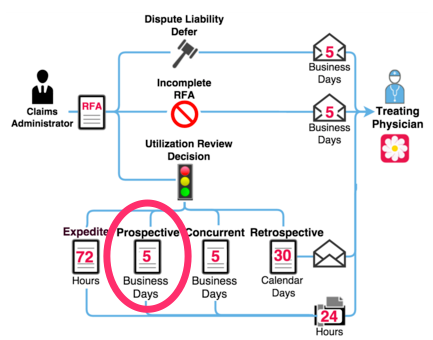
Prospective Review Required Timeline
Per regulation 9792.9.1(c)(3), a utilization review decision for a prospective RFA is due within 5 business days after receipt of the completed DWC Form RFA.
For a prospective RFA, the claims administrator must communicate the decision to the requesting physician within 24 hours of making the decision.
Written notice of the decision is required within 2 business days of the prospective review decision.
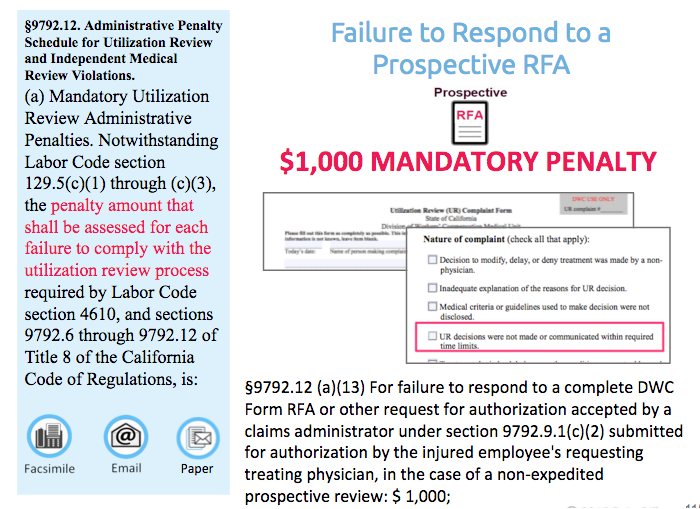
Perspective Review Penalty
If a claims administrator fails to respond to a prospective RFA, regulation 9792.12(a) mandates that the mandatory penalty is $1,000 for each failure.
California Code of Regulations (CCR)
§ 9792.6.1 Utilization Review Standards - Definitions - On or After January 1, 2013
§ 9792.9.1 Utilization Review Standards - Timeframe, Procedures and Notice - On or After January 1, 2013
§ 9792.12 Administrative Penalty Schedule for Labor Code § 4610 Utilization Review Violations
DaisyBill Resources
Daisy News: Your Request for Authorization (RFA) Questions Answered
For more information about California’s workers’ comp electronic billing, watch DaisyBill’s free, information-packed webinars.