California Labor Code Article 2. § 4603.2(e) stipulates that improper payment for compliant medical bills requires an appeal using the following process.
Appeal Process |
|
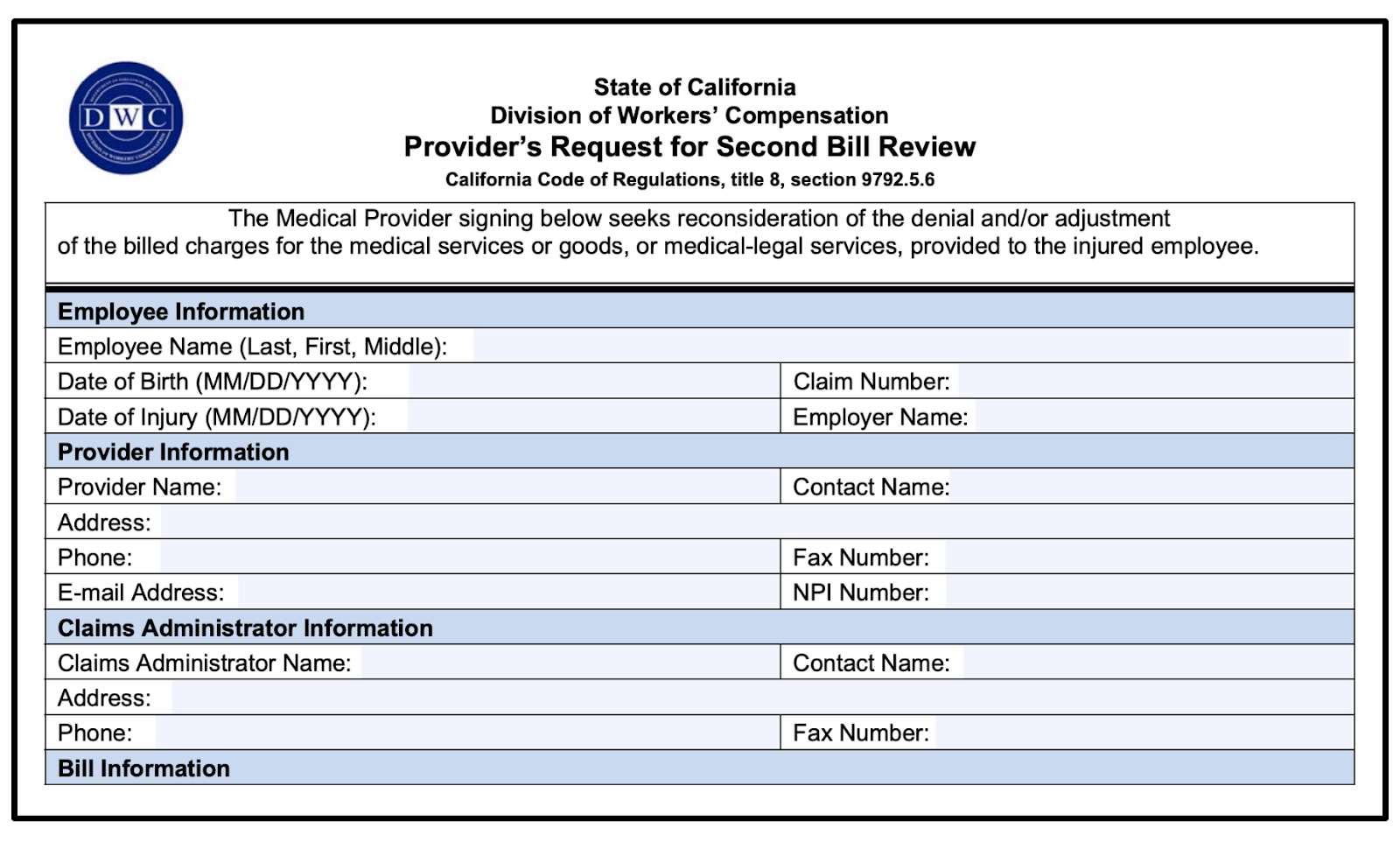
Step 1: Provider - Second Bill Review (DWC Form SBR-1)
Appeal Type |
Regulations |
Timeline |
Form |
Request for Second Review (SBR) |
9792.5.4. Second Review and Independent Bill Review – Definitions |
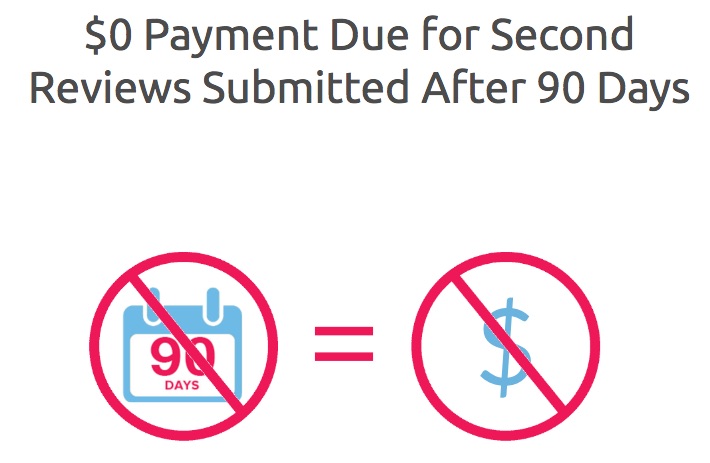
File within 90 Days of initial EOR receipt |
After a provider receives reimbursement and Explanation of Review (EOR); if the provider disputes the amount of payment, needs to submit a timely Second Bill Review (SBR) appeal within 90 days of receiving the EOR from the claims administrator. This process allows providers to dispute the reimbursement amount made by the claims administrator “in conjunction with the payment, adjustment, or denial of the initially submitted bill, if a proof of service accompanies the explanation of review” on a bill for medical treatment services or goods rendered, under California Code of Regulations § 9792.5.5.
For more information on reasons for filing a Second Review appeal and the language to use, refer to daisyBill’s Reasons to File for Second Review article.
Submitting Form SBR-1
Requests for bill review must be transmitted using the same method as the initial bill. So, when an initial bill is transmitted via paper (non-electronically), the provider must also transmit the second review non-electronically via paper.
DWC Form SBR-1 is optional for paper billing.
Paper Initial Bill
Second review may be requested with either the SBR-1 Form as a cover page or on the initially reviewed bill marked, in accordance with C.C.R. section 9792.5.5(c)(1). Based on the bill type, modify the bill with the correct designator in the correct box on the bill.
Bill Type |
Modified Initial Billing |
CMS-1500 |
Box 10d: BGW3 |
UB-04 |
Box 18-28: BGW3 |
ADA Dental Claim Form |
Field 1: “Request for Second Review” |
NCPDP WC/PC Claim Form |
“Request for Second Review” |
When submitting a modified bill, C.C.R. § 9792.5.5(d)(2) requires providers to include the following supporting information:
- The date of the explanation of review
- the claim number or other unique identifying number provided on the explanation of review
- The item and amount in dispute
- The additional payment requested and the reason therefore
- The additional information provided in response to a request in the first explanation of review or any other additional information provided in support of the additional payment requested
This information is included on the SBR-1 form. If you are not using the SBR-1 form, submit this information as a supporting document with the modified initial bill.
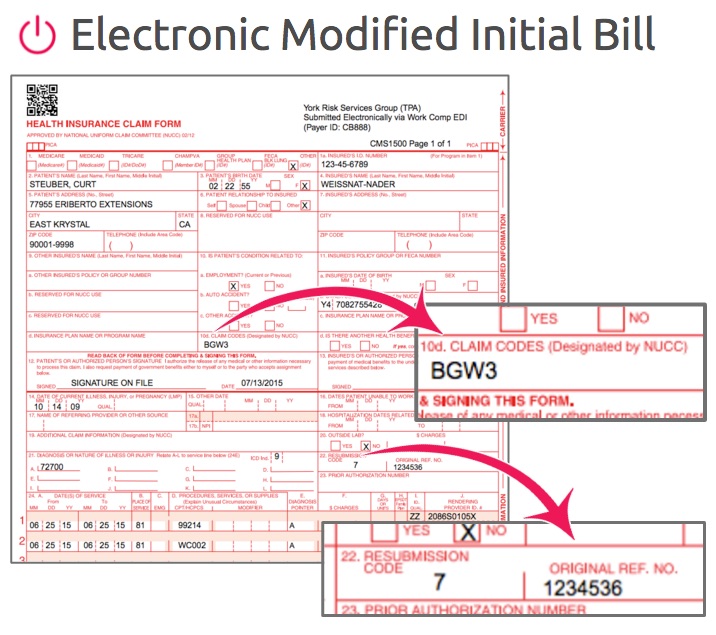
Electronic Initial Bill
If the initial bill is submitted electronically, the second review must also be submitted electronically. For electronic initial billing, the second review must be submitted as an electronic modified bill and contain the required additional information (listed above).
Per the DWC Electronic Medical Billing and Payment Companion Guide, for the electronic CMS-1500, the text “BGW3” must populate box 10d of the CMS1500. Additionally, the number 7 and the original reference number used on the initial bill must populate box 22.
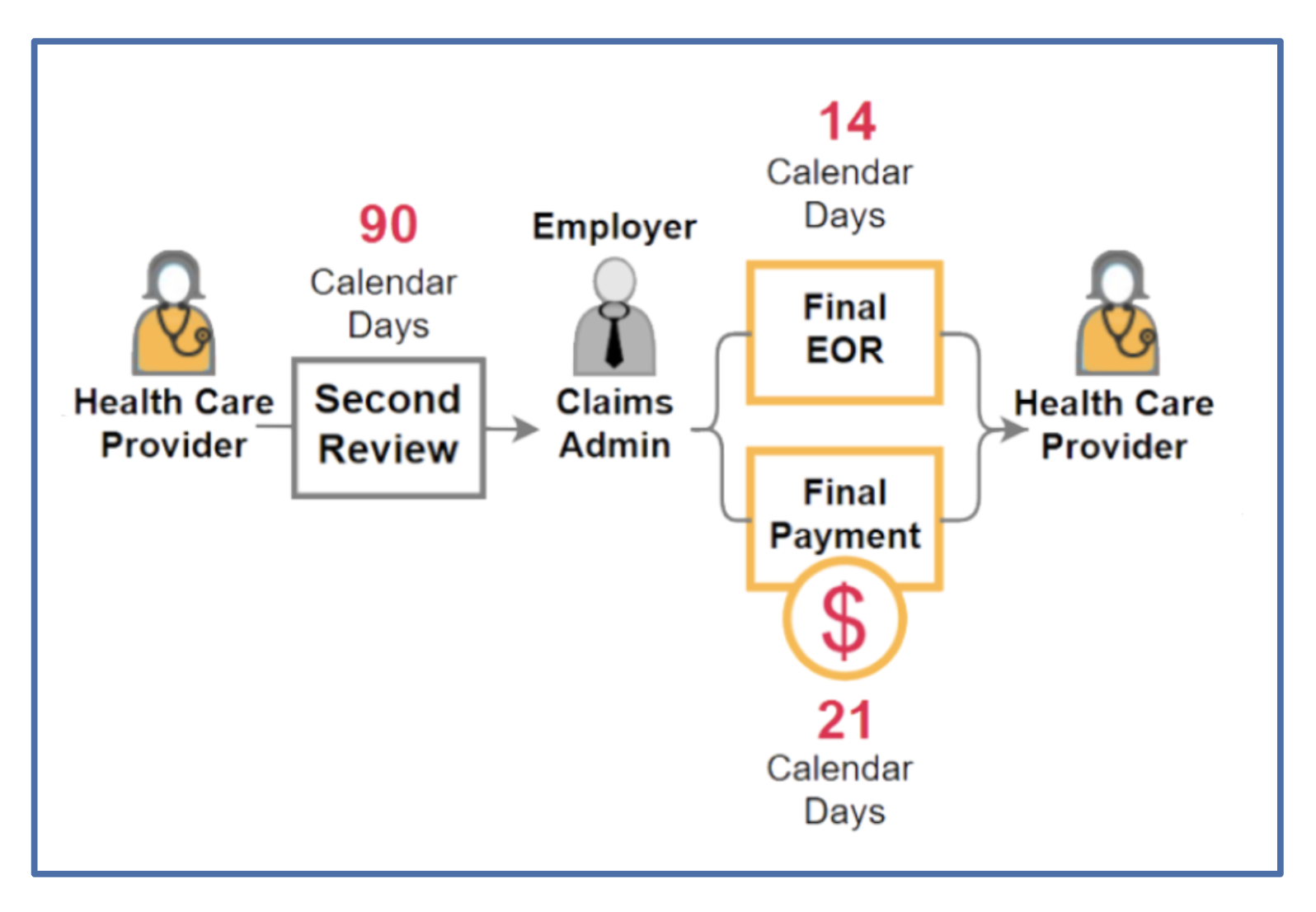
Step 2: Payor - Final EOR and Payment
California Labor Code § 4603.2(e)(2) protects employees and employers from liability for disputed payments if a provider fails to file an SBR within 90 days.
If a provider does file a compliant SBR request within the required 90 day period, the claims administrator has 14 calendar days to conduct a review of the bill and issue a Final Explanation of Review in response.
Final EORs, per C.C.R. § 9792.5.5(g), must include:
- A written final determination on each of the items or amounts in dispute
- All the information that is required to be set forth in an explanation of review under Labor Code section 4603.3
- An explanation of the time limit to raise any further objection regarding the amount paid for services and how to obtain independent bill review
Providers should then receive payment for the remaining sum due within 21 calendar days of the claims administrator receiving the request.
NOTE: The 14-day time limit for responding to a request for the Second Review appeal may be extended by mutual written agreement between the provider and the claims administrator.
Step 3: Provider - Independent Bill Review (DWC Form IBR-1)
Appeal Type |
Regulations |
Timeline |
Form |
Fee |
Independent Bill Review (IBR) |
30 days of the date of service of the final written determination |
$180 |
Once a claims administrator produces a Final EOR, and the provider is still unsatisfied with the payment amount, the provider has 30 days to file for independent bill review (IBR) with a third party entity designated by the State of California. The DWC designated Maximus Federal Services as the entity responsible for independent bill review.
The Independent Bill Review process is exclusively reserved for disputes over payment amount for medical treatment or medical-legal bills.
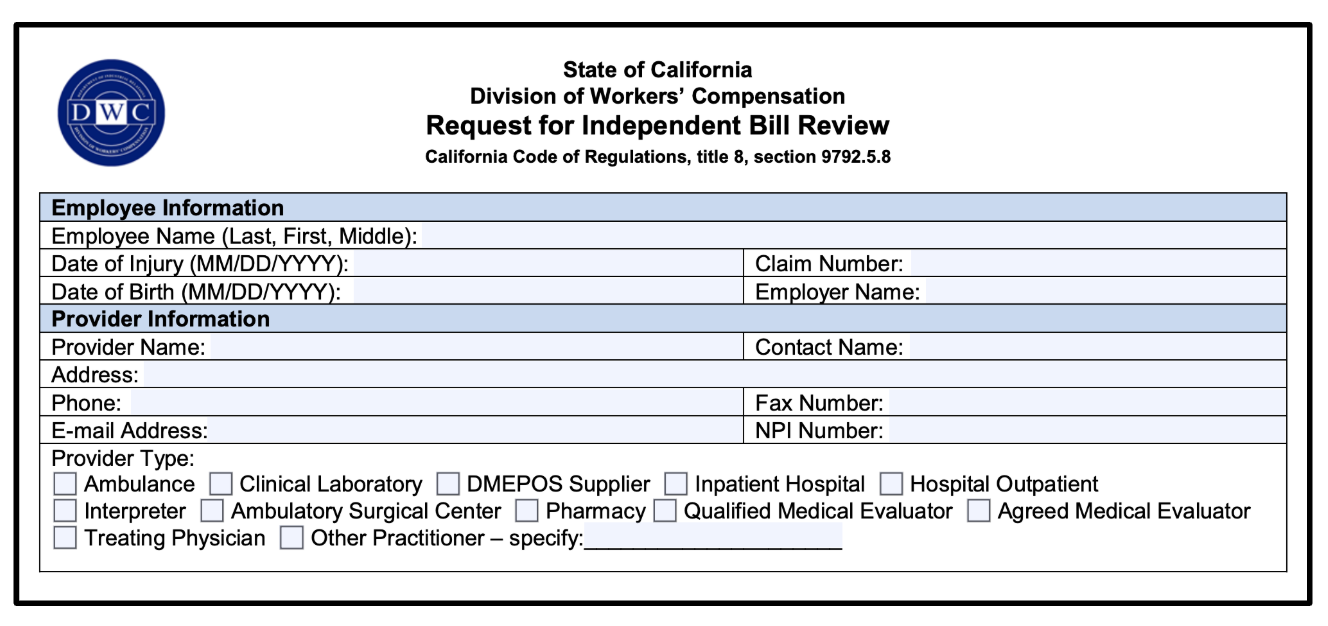
FIling for Independent Bill Review (Form IBR-1)
To file for IBR, in accordance with § 9792.5.7(d)(1), the request for independent bill review shall be made by either:
- Completing and electronically submitting the online Request for Independent Bill Review form on the DWC website and paying the required fee of $335 electronically.
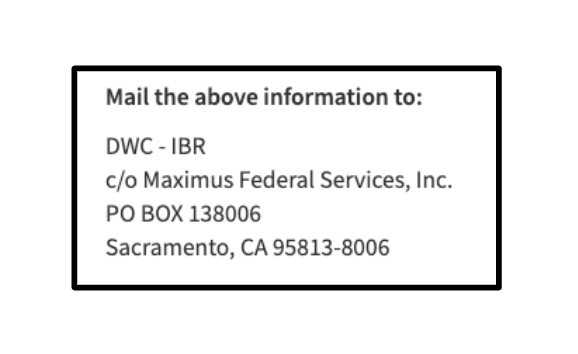
- Mailing the Request for Independent Bill Review form (DWC Form IBR-1) with a check or money order for the required fee of $180, and any required supporting documentation to Maximus.
NOTE: The DWC announced a reduction in IBR fees in 2020; the cost for an IBR Request is $180, down from $195 and NOT the $335 price listed on the form.
C.C.R § 9792.5.7(d)(2) requires providers to submit the following supporting documentation with DWC Form IBR-1:
- The original billing itemization
- Any supporting documents that were furnished with the original billing
- If applicable, the relevant contract provisions for reimbursement rates under Labor Code section 5307.11
- The explanation of review that accompanied the claims administrator's response to the original billing
- The provider's request for second review of the claims administrator's original response to the billing
- Any supporting documentation submitted to the claims administrator with that request for second review
- The final written determination of the second review (explanation of review) issued by the claims administrator to the provider
Consolidating IBR Requests
Requests for IBR may be consolidated. According to the form’s instructions, a provider may request that multiple (up to twenty) requests for IBR be consolidated into one. The DWC or IBRO will then determine that the requests do, in fact, involve “common issues of law and fact or the delivery of similar or related services” if:
- requests for IBR by a single provider involving multiple dates of medical treatment services involve one injured employee, one claims administrator, and one billing code under an applicable fee schedule or, if applicable, under a contract for reimbursement rate, and the total amount in dispute does not exceed $4,000.00; or
- requests for IBR by a single provider involving multiple billing codes under applicable fee schedules or, if applicable, under a contract for reimbursement rates, with no limit on the total dollar amount in dispute and involves one injured employee, one claims administrator, and one date of medical treatment service.
Additional Information
California Code of Regulations § 9792.5.5
California Labor Code § 4603.2
California Code of Regulations § 9792.5.7
California e-billing Regulations
daisyBill Resources
Webinar: Request for Second Review
Webinar: Second Review Strategy Kit, Part I
Webinar: Second Review Strategy Kit, Part II
daisyBill Solution
Every request for Second Review submitted from daisyBill is compliantly submitted using both a completed DWC Form SBR-1, as well as a compliant modified CMS-1500.