After a bill submitted by a provider is accepted by the claims administrator and the provider receives an Explanation of Review (EOR) or the claims administrator denies payment; providers retain the option of requesting Second Bill Review (SBR) within 90 days. This process allows providers to dispute the reimbursement amount made by the claims administrator “in conjunction with the payment, adjustment, or denial of the initially submitted bill, if a proof of service accompanies the explanation of review” on a bill for medical treatment services or goods rendered, under California Code of Regulations § 9792.5.5.
This article outlines what language to use when filing a Request for SBR for incorrectly denied or underpaid original medical bills and includes appropriate IBR decisions as supporting documentation.
Reason to File a Request for Second Review | |
|
Incorrect Denial |
|
Incorrect Reimbursement |
|
For more information on Filing a Request for Second Review, please review daisyBill’s article on the Disputed Payment Appeal Process in California. To store language for Request for Second Review reasons within daisyBill software, please refer to the Second Bill Review Reasons Help Article.
Correcting a Coding Error on a Bill
Fee Schedule |
CPT Codes |
Payable |
Any |
Any |
Yes |
If a provider determines that a bill was denied due to a coding error, daisyBill advises filing a Second Review using the language and including the IBR decisions included in the following table as supporting documentation.
Even if the bill was submitted with errors and has not been denied yet, daisyBill recommends requesting Second Review. There are processes for submitting corrected electronic and non-electronic original bills. However, both processes are unreliable. Be sure to wait for the Explanation of Review (EOR) from the claims administrator before initiating the second review appeal.
NOTE: If you mistakenly left out a procedure code(s) or under-reported the number of units, simply submit an original bill ONLY for the missing procedure code(s) or the additional units of service.
Theoretically, providers can resubmit corrected bills. Instructions for doing so are located in the DWC Medical Billing and Payment Guide for non-electronic bills, and the Electronic Billing and Payment Companion Guide for electronic bills; however, the guidelines for bill resubmission are contradictory and the provider may not know if the EOR has already been sent by the claims administrator, which renders the corrected bill invalid. This option is far simpler and more likely to result in correct payment. For more detail, see our blog.
Attachment |
Recommendation |
Reason |
Code XXX was denied due to the following denial reason: XXX. The practice incorrectly submitted the original bill with Code XXX. The correct code for the service is XXX.
Please reprocess this bill using the correct Code XXX. Per CCR §9792.5.5 (d)(1) when submitting a Second Review, "No new dates of service or additional billing codes may be included."
Optional: Further, Maximus IBR decisions have ruled that the protocol for correcting a processed bill is to submit a Second Review with the correction. |
Back to Top
Denial Incorrect: Automatically Authorized Services Denied
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Any |
Any |
Yes |
This service requires prior authorization and none was identified |
If a claims administrator denies payment for automatically authorized services, daisyBill advises filing a Second Review using the language and including the IBR decisions included in the following table as supporting documentation.
Unlike standard authorization, the claims administrator has no input in determining the necessity or appropriateness of the treatment. The claims administrator cannot modify or deny automatically authorized treatment nor can authorization be rescinded for any reason.
NOTE: Even if the RFA, DLSR, or original bill is untimely submitted, the claims administrator must pay for automatically authorized services rendered. While Labor Code § 4610 requires the provider to submit an RFA within 5 days of treatment, and to submit the original bill within 30 days (for non-emergency treatment) or 180 days (for emergency treatment), failure to meet these deadlines is not grounds for non-payment.
For more information on appealing denial of automatically authorized services, review this blog post.
Attachment |
Recommendation |
Reason |
The attached request for payment meets the requirements for authorization per Labor Code § 4610(b) which became effective for all dates of service on or after 1/1/2018.
Treatment and/or emergency services were provided and all required conditions were met, as follows:
Labor Code § 4610(b) makes no provision for non-payment for services authorized thereunder, whether or not the following documentation has been timely submitted:
|
Supporting Documents |
Any documentation that substantiates the treatment’s eligibility for automatic authorization |
Back to Top
Denial Incorrect: No Authorization
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Any |
Any |
Yes |
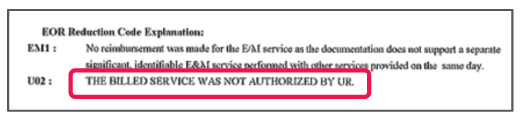
The billed service was not authorized by UR. |
For incorrectly denied or underpaid original bills, daisyBill advises filing a Second Review using the language and including the IBR decisions included in the following table as supporting documentation.
Attachment |
Recommendation |
Reason |
UR authorized all billed services. Please reprocess this bill and issue payment. Documented authorization submitted with original bill.
The authorization is included with this SBR-1 Form.
Optional: Attached is a copy of an OVERTURN IBR Decision indicating this incorrect denial will be overturned when reviewed by IBR. |
Back to Top
Denial Incorrect: PTP Evaluation & Management (E/M) Visit
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Physician Services |
99213-99215 |
Yes |
This service requires prior authorization and none was identified. |
99203-99205 |
For incorrectly denied original bills, daisyBill advises filing a Second Review using the language and including the IBR decisions included in the following table as supporting documentation.
For help determining the correct level of E/M code and documentation, read daisyBill’s Helpful Resources article on How to Determine the Correct E/M Code.
Attachment |
Recommendation |
Reason |
Evaluation and Management visits do not require prior authorization when performed by the designated Primary Treating Physician (PTP).
Optional: Attached is a copy of an OVERTURN IBR decision indicates that this reimbursement will be overturned when reviewed by IBR. |
Back to Top
Denial Incorrect: PPO / Network Reduction Incorrectly Applied
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Any |
Any |
Yes |
Reduction in accordance with _____ Contract.
This charge was adjusted to comply with the rate and rules of the contract indicated. |
Preferred Provider Organization (PPO) and Medical Provider Network (MPN) contracts are rife with abuse, as daisyBill documents in the Discount Contracts blog series. Insurance companies sometimes try to force lower reimbursement rates on providers by processing lower rates than those outlined in agreements with providers. Providers should keep all discount contracts on file to verify that discounts are correctly applied and be ready to appeal any errors.
For incorrectly denied bills citing a PPO or Network discount/reduction, daisyBill advises filing a Second Review using the language and including the IBR decision included in the following table as supporting documentation.
Attachment |
Recommendation |
Reason |
An incorrect PPO discount rate was used to calculate reimbursement.
Contracted rate is ___%
Accordingly, please review this bill for additional payment per OMFS.
Optional: Attached is a copy of an OVERTURN IBR Decision indicating this incorrect PPO discount will be overturned when reviewed by IBR. |
Back to Top
Denial Incorrect: 99358 Denied As Not Reimbursable
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Physician Services |
99358 |
Yes |
Does not fall under the fee schedule guidelines of a reimbursable report. |
99359 |
When a medical bill is incorrectly denied reimbursement for CPT Codes 99358 or 99359, daisyBill advises filing a Second Review using the language included in the following table.
For more information on codes 99358 and 99359, read daisyBill’s 5 Point Checklist for CPT Codes 99358 and 99359 blog post.
Attachment |
Recommendation |
Reason |
The AMA CPT Definition of 99358 is as follows: Prolonged evaluation and management service before and/or after direct patient care; first hour. For dates of service on or after 3/1/2017 RBRVS indicate 99358 with a payment status code of "A" payable.
Please pay accordingly. |
Back to Top
Incorrect Reimbursement: Physical Medicine / Chiropractic / Acupuncture
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Physician Services |
Physical Medicine / Chiropractic / Acupuncture Multiple Procedure Payment Reduction; Pre-Authorization for Specified Procedure / Modality Services |
Yes |
Maximum units exceeded. |
For underpaid Physical Medicine / Chiropractic / Acupuncture bills, daisyBill advises filing a Second Review using the language and including the IBR decisions included in the following table as supporting documentation.
For help with Multiple Procedure Payment Reductions, review daisyBill’s article (and video!) covering Multiple Procedure Payment Reduction (MPPR) for Physical Medicine.
Attachment |
Recommendation |
Reason |
MUE incorrectly cited as reason for $0 reimbursement. § 9789.12.13 Correct Coding Initiative.
(c) Medically Unlikely Edits are published by CMS on its website at: https://www.cms.gov/Medicare/Coding/NationalCorrectCodInitEd/MUE.html document “Practitioner Services MUE Table.” See section 9789.19 for the adopted version of the Practitioner Services MUE Table, by date of service. |
Back to Top
Incorrect Reimbursement: CCI Edit
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Any |
Any |
Yes |
No separate payment was made because the value of the service is included within the value of another service performed on the same day. |
When a CCI Edit is incorrectly cited as a reason for $0 reimbursement, daisyBill advises filing a Second Review using the language and including the IBR decisions included in the following table as supporting documentation.
For more information on CCI Edits and MUEs please refer to daisyBill’s Correct Coding Initiative article.
Attachment |
Recommendation |
Reason |
CCI Edit incorrectly cited as reason for $0 reimbursement. § 9789.12.13 Correct Coding Initiative. (d) Physician NCCI Edits are published by CMS on its website at: https://www.cms.gov/Medicare/Coding/NationalCorrectCodInitEd/index.html. See section 9789.19 for the adopted version of the Physician CCI Edits, by date of service.
Optional: Attached is a copy of an OVERTURN IBR Decision indicating this incorrect denial will be overturned when reviewed by IBR. |
Back to Top
Incorrect Reimbursement: Evaluation & Management (E/M) Downcoding
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Physician Services |
99213-99215 |
Yes |
The documentation does not support the level of service billed. Reimbursement was made for a code that is supported by the description and documentation submitted with the billing. |
99203-99205 |
For underpaid medical bills, daisyBill advises filing a Second Review using the language and including the IBR decisions included in the following table as supporting documentation.
For help determining the correct level of E/M code and documentation, read daisyBill’s Helpful Resources article on How to Determine the Correct E/M Code.
Attachment |
Recommendation |
Reason (example of 99214 incorrectly downcoded to 99213) |
This CPT was paid at a lower rate than documented in the provided medical records. Per the 1995 AMA CPT guidelines, two of three key components (history, examination, and medical decision making) determine established patient evaluation and management (E/M) level. In the case where counseling and/or coordination of care dominates the physician/patient encounter, time is the controlling factor to qualify for a particular level of E/M service.
The medical records document the time spent face-to-face with the patient, a detailed history was done, review of previous records and recently obtained records and required medical decision making. These factors indicate that 99214 is the appropriate level of reimbursement.
Optional: Attached is a copy of an OVERTURN IBR decision, including the guidelines used to evaluate appropriate 99214 E/M level. This IBR decision indicates that this reimbursement will be overturned when reviewed by IBR. |
Back to Top
Incorrect Reimbursement: No PPO / Network Reduction
Fee Schedule |
CPT Codes |
Payable |
EOR Denial Reason |
Any |
Any |
Yes |
Reduction in accordance with _____ Contract.
This charge was adjusted to comply with the rate and rules of the contract indicated. |
Preferred Provider Organization (PPO) and Medical Provider Network (MPN) contracts are rife with abuse, as daisyBill documents in the Discount Contracts blog series. Insurance companies sometimes try to force lower reimbursement rates on providers by processing “contract” discounts when no contract actually exists or the sale of a contract to another agency was not properly disclosed. In either case, these discounts often do not apply and should be appealed. Providers should keep all discount contracts on file and readily verifiable to avoid taking reduced rates they never agreed to.
For underpaid bills incorrectly citing a PPO or Network discount/reduction, daisyBill advises filing a Second Review using the language and including the IBR decision included in the following table as supporting documentation.
Attachment |
Recommendation |
Reason |
This bill payment was incorrectly discounted citing a “PPO Discount”.
Despite requesting proof of PPO contract, to date, no proof of PPO contract has been received.
This practice and provider do NOT have a PPO contract or agreement authorizing this payment discount. Accordingly, please review this bill for additional payment per OMFS.
Optional: Attached is a copy of an OVERTURN IBR Decision indicating this incorrect PPO discount will be overturned when reviewed by IBR. |
Supporting Documents |
Letter to claims/contract administrator requesting proof of PPO contract |
daisyBill Resources
Webinar: Request for Second Review
Webinar: Second Review Strategy Kit, Part I
Webinar: Second Review Strategy Kit, Part II
daisyBill Solution
Every request for Second Review submitted from daisyBill is compliantly submitted using both a completed DWC Form SBR-1, as well as a compliant modified CMS 1500.