Texas Labor Code Section 413.031 stipulates that providers “denied payment or paid a reduced amount for the medical service rendered” are “entitled to a review of a medical service provided or for which authorization of payment is sought.”
Cause |
Appeal Type |
Regulation |
Timeline |
Form |
Incorrect Payment Amount |
Medical Fee Dispute Resolution Request |
12 months |
Definition
The Texas Administrative Code defines a medical fee dispute as a “dispute that involves an amount of payment for non-network health care [emphasis ours] rendered to an injured employee that has been determined to be medically necessary and appropriate for treatment of that injured employee's compensable injury.”
Disputes arising about insurance carrier reduction or denial of bills or regarding the results of audits which requires a provider to refund insurance carriers
Completing the Form
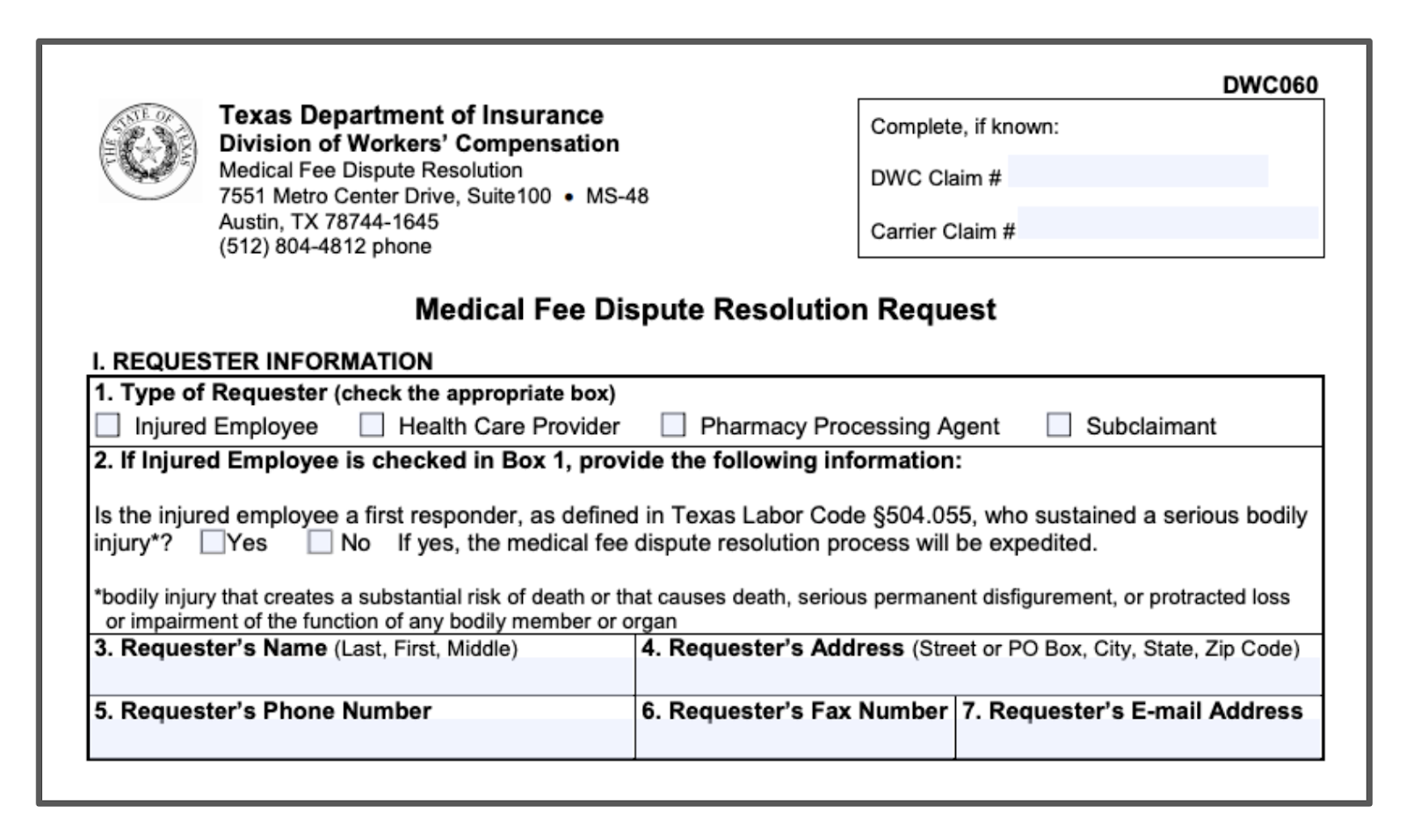
The Texas Department of Insurance requires providers to complete Parts I, II, and V of the Medical Fee Dispute Resolution (MFDR) Form (DWC Form-060) and to list all dates of service for the medical bills in dispute.
Supporting Document Requirements
The Texas Administrative Code, Rule §133.307(a)(2), requires the following supporting documentation to be submitted with MFDR Form for an appeal:
- the name, address, and contact information of the requestor;
- the name of the injured employee;
- the date of the injury;
- the date(s) of the service(s) in dispute;
- the place of service;
- the treatment or service code(s) in dispute;
- the amount billed by the health care provider for the treatment(s) or service(s) in dispute;
- the amount paid by the workers' compensation insurance carrier for the treatment(s) or service(s) in dispute;
- the disputed amount for each treatment or service in dispute;
- a paper copy of all medical bill(s) related to the dispute, as originally submitted to the insurance carrier in accordance with this chapter and a paper copy of all medical bill(s) submitted to the insurance carrier for an appeal in accordance with §133.250 of this chapter (relating to General Medical Provisions);
- a paper copy of each explanation of benefits (EOB) related to the dispute as originally submitted to the health care provider in accordance with this chapter or, if no EOB was received, convincing documentation providing evidence of insurance carrier receipt of the request for an EOB;
- when applicable, a copy of the final decision regarding compensability, extent of injury, liability and/or medical necessity for the health care related to the dispute;
- a copy of all applicable medical records related to the dates of service in dispute;
- a position statement of the disputed issue(s) that shall include:
- the requestor's reasoning for why the disputed fees should be paid or refunded,
- how the Labor Code and division rules, including fee guidelines, impact the disputed fee issues, and
- how the submitted documentation supports the requestor's position for each disputed fee issue;
- documentation that discusses, demonstrates, and justifies that the payment amount being sought is a fair and reasonable rate of reimbursement in accordance with §134.1 of this title (relating to Medical Reimbursement) or §134.503 of this title (relating to Pharmacy Fee Guideline) when the dispute involves health care for which the division has not established a maximum allowable reimbursement (MAR) or reimbursement rate, as applicable;
- if the requestor is a pharmacy processing agent, a signed and dated copy of an agreement between the processing agent and the pharmacy clearly demonstrating the dates of service covered by the contract and a clear assignment of the pharmacy's right to participate in the MFDR process. The pharmacy processing agent may redact any proprietary information contained within the agreement; and
- any other documentation that the requestor deems applicable to the medical fee dispute.
For additional information related to reporting please refer to daisyBill’s Texas Billing Guide.
Filing the Form
To file the form, requestors must send or deliver two copies to the TDI-MFDR Section at the following address:
Requests must be filed within a year of the date of service in dispute, unless exempted, and will be considered to be filed on the date that the DWC receives the request.
Timeline Exemptions
According to Texas Administrative Code, Rule §133.307(c)(1)(B), Requests must be filed within a year of the date of service in dispute, unless:
– a related compensability, extent of injury, or liability dispute under Labor Code Chapter 410 has been filed, the medical fee dispute shall be filed not later than 60 days after the date the requestor receives the final decision, inclusive of all appeals, on compensability, extent of injury, or liability;
– a medical dispute regarding medical necessity has been filed, the medical fee dispute must be filed not later than 60 days after the date the requestor received the final decision on medical necessity, inclusive of all appeals, related to the health care in dispute and for which the insurance carrier previously denied payment based on medical necessity; or
– the dispute relates to a refund notice issued pursuant to a division audit or review, the medical fee dispute must be filed not later than 60 days after the date of the receipt of a refund notice.
Required Form
The Texas Department of Insurance requires providers to file DWC Form-060, the Medical Fee Dispute Resolution (MFDR) Form for disputed payment appeals.
daisyBill Solution
Stay up-to-date on the latest developments in Workers’ Compensation medical billing by subscribing to daisyBill’s email list.