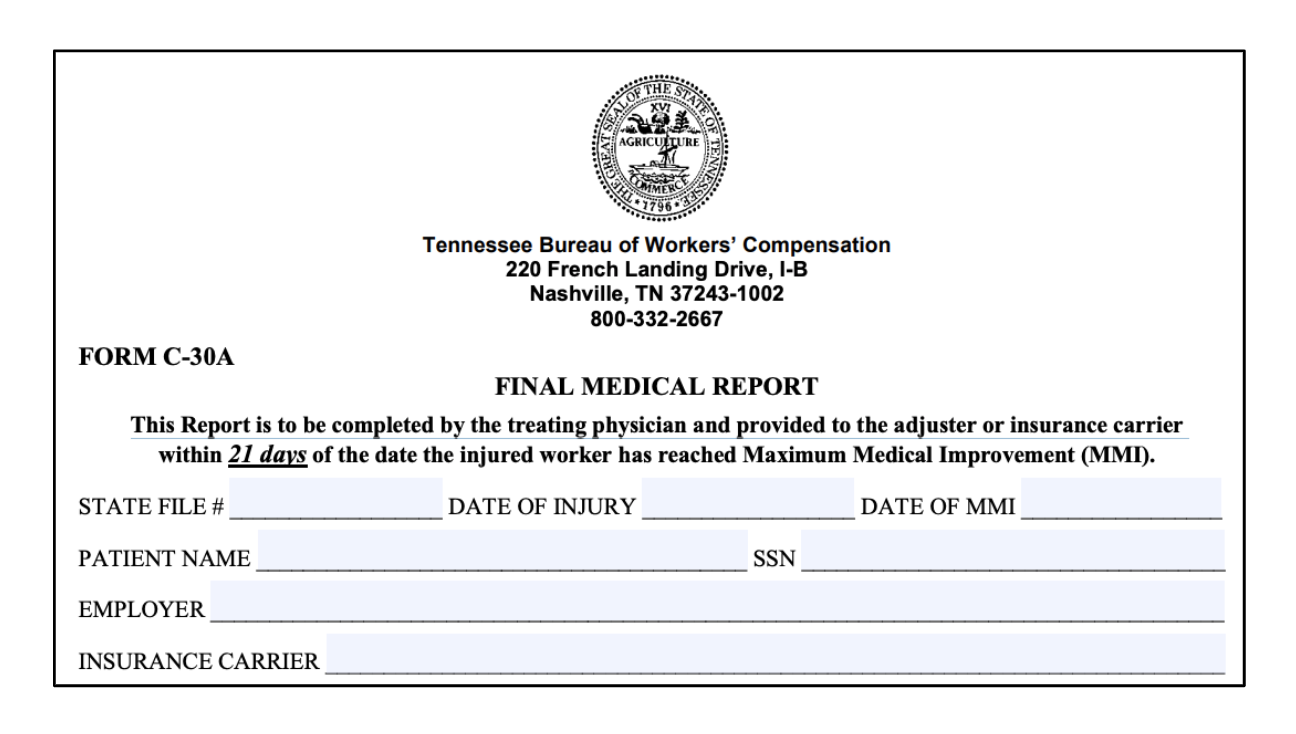
Tennessee’s Rules for Medical Payments (Rule 0800-02-17-.15) require health care providers to file a Final Medical Report with the employer within 21 days of the authorized treating physician determining that the employee has reached maximum medical improvement (MMI) regarding the condition or injury for which the physician has provided treatment. If the work-related incident caused multiple injuries to an employee, physicians should take care to determine MMI and impairment ratings only for those injuries which the physician is treating. The employer must then submit a fully completed to each party—including the Bureau of Workers’ Compensation—within 30 calendar days of the MMI date.
Reimbursement
The authorized treating physician is required and responsible for submitting the report to the employer using CPT® code 99455, but “shall receive payment of no more than $250.00 for these services.”
NOTE: Physicians should be careful to document consultation with the applicable AMA Guides™ to ensure appropriate reimbursement.
The report itself is exempt from the rule prohibiting charges for filing required medical reports with the Bureau. Providers are entitled to reimbursement for the Final Medical Report, “not to exceed $10.00 for reports twenty (20) pages or less in length, and twenty-five (25) cents per page after the first twenty pages,” and using procedure code WC103.
Form
Final Medical Reports must be completed and filed on Form C-30A (PDF). The form requires the authorized physician to determine the date of MMI and to determine the Impairment Rating of the injury in question using the 6th Edition of the AMA Guides.
For additional information on reporting please refer to daisyBill’s Tennessee Billing Guide.
daisyBill Solution
Stay up-to-date on the latest developments in Workers’ Compensation medical billing by subscribing to daisyBill’s email list.