The CMS-1500 (HCFA) Form is used by healthcare providers and professionals to file original workers' compensation medical bills and reports in New York.
Article Contents |
Navigation Link |
CMS-1500 Form |
|
Supporting Documentation |
|
Timely Filing |
|
Filling out the Form |
CMS-1500 Initiative
The New York State Workers’ Compensation Board has implemented the CMS-1500 Initiative, adopting the form to reduce administrative burden in the workers’ compensation medical billing process for providers. While the reporting requirements themselves will not change, they may now be fulfilled using the CMS-1500 Form and an accompanying narrative.
The following table lists the forms the Board replaced with the CMS-1500 Form:
Form |
Name |
Forms C-4, EC-4 |
Doctor's Initial Report |
Form C-4.1 |
Continuation to Carrier/Employer Billing Section |
Forms C-4.2, EC-4.2 |
Doctor's Progress Report |
Forms C-4AMR, EC-4AMR |
Ancillary Medical Report |
Form EC-4NARR |
Doctor's Narrative Report |
Forms OT/PT-4, EOT/PT-4 |
Occupational / Physical Therapist's Report |
Form PS-4 |
Psychologist's Report |
Form C-5 |
Ophthalmologist's Report |
Required Billing Documentation
For a complete CMS-1500, the Workers’ Compensation Board requires providers to submit a Narrative Report with all CMS-1500 Forms.
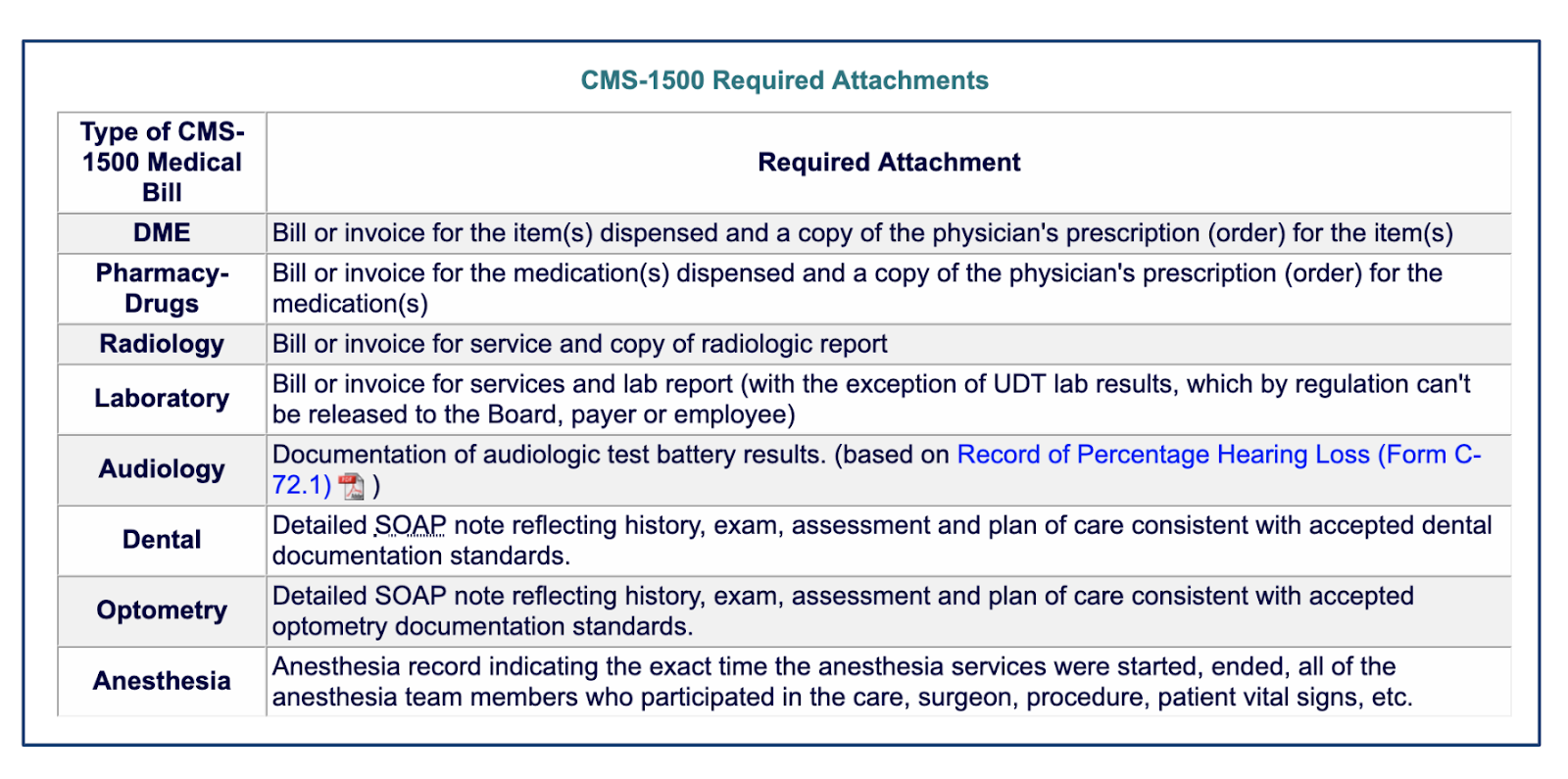
The following supporting documentation is also required, when applicable:
CMS-1500 Initiative. (2019, July 24) Retrieved from http://www.wcb.ny.gov/CMS-1500/requirements.jsp
For additional information related to reporting please refer to daisyBill’s New York Billing Guide.
Timely Filing
CMS-1500 Forms must be filed within the following timelines after the date of service for all professional services rendered in New York:
Form |
Timely Filing |
Workers’ Comp Board |
Rule |
Initial Medical Report on CMS-1500 |
Within 48 hours of first treatment. |
||
Subsequent Medical Report on CMS-1500 |
15 days after first treatment, and thereafter for continuing treatment;
|
||
Medical Bill |
Within 120 days from the date of service. |
— |
CMS-1500 Form Instructions
The state of New York requires providers to compliantly complete the CMS-1500 Form as detailed in the following tables.
For additional information, review the complete NUCC Manual:
1500 Health Insurance Claim Form Reference Instruction Manual for Form Version 02/12
Items 0 through 10
CMS-1500 Box # |
CMS-1500 (02/12) Field Description |
New York Fields from form C-4 |
New York Workers' Compensation Requirements (Required/ Situational/ Optional / Not Applicable) |
New York Workers' Compensation Instructions |
0 |
CARRIER NAME AND ADDRESS |
D-1 Employer's Insurance Carrier D-2 Carrier Code D-3 Carrier Address |
R |
Carrier Name, Address, State, Zip code |
1 |
MEDICARE, MEDICAID, TRICARE, CHAMPVA, GROUP HEALTH PLAN, FECA, BLACK LUNG, OTHER |
R |
Enter 'X' in Box Other. [SELECT ONE BOX] |
|
1a |
INSURED’S I.D. NUMBER |
A-5 Carrier Case # |
O |
Enter the claimant's nine digit SSN number. |
2 |
PATIENT’S NAME (Last Name, First Name, Middle Initial) |
A-1 Last Name |
R |
|
3 |
PATIENT’S BIRTH DATE, SEX |
A-8 Date of Birth |
R |
Date = [MM DD YYYY] |
4 |
INSURED’S NAME (Last Name, First Name, Middle Initial) |
R |
For Workers' Compensation, the Insured is the Employer. Enter the name of the Employer. |
|
5 |
PATIENT’S ADDRESS (No., Street), CITY, STATE, ZIP CODE, TELEPHONE |
A-6 Number and Street |
R |
|
6 |
PATIENT RELATIONSHIP TO INSURED |
R |
Enter 'X' in Box 'Other'. [SELECT ONE BOX] |
|
7 |
INSURED'S ADDRESS (No., Street), CITY, STATE, ZIP CODE, TELEPHONE |
R |
||
8 |
RESERVED FOR NUCC USE |
R |
Must have: Unique document ID# [CMS1500 document ID#]; Unique narrative document ID# [Narrative ID#] Carrier acknowledgement date [YYYY-MM-DD]; Carrier W#; XML partner name or ID# |
|
9 |
OTHER INSURED'S NAME (Last Name, First Name, Middle Initial) |
S |
Required if applicable. |
|
9a |
OTHER INSURED'S POLICY OR GROUP NUMBER |
O |
Enter Claimant's WCB Claim Number if known. |
|
9b |
RESERVED FOR NUCC USE |
N |
||
9c |
RESERVED FOR NUCC USE |
N |
||
9d |
INSURANCE PLAN NAME OR PROGRAM NAME |
S |
Required if applicable. |
|
10a |
IS PATIENT'S CONDITION RELATED TO: EMPLOYMENT |
R |
Enter 'X' in Box 'YES'. |
|
10b |
IS PATIENT'S CONDITION RELATED TO: AUTO ACCIDENT _ PLACE (State) |
N |
||
10c |
IS PATIENT'S CONDITION RELATED TO: OTHER ACCIDENT |
N |
||
10d |
CLAIM CODES (Designated by NUCC) |
S |
Note: Do not use condition codes when submitting appeals to a bill. The HP-1 form should be used to handle appeals. |
Top of Section
Items 11 through 20
CMS-1500 Box # |
CMS-1500 (02/12) Field Description |
New York Fields from form C-4 |
New York Workers' Compensation Requirements (Required/ Situational/ Optional / Not Applicable) |
New York Workers' Compensation Instructions |
11 |
ISURED'S POLICY GROUP OR FECA NUMBER |
O |
For WC, the "insured" is the employer. The provider may enter the employer's WC insurance policy number |
|
11a |
INSURED'S DATE OF BIRTH, SEX |
N |
||
11b |
OTHER CLAIM ID (Designated by NUCC)(left of vertical dotted line) |
R |
Required if known. Enter qualifier Y4. Required if known. Enter WC claim number assigned by the claims administrator. If claim is not yet assembled enter the value of "Unknown". This item requires these values and cannot be left blank or may result in the bill being rejected. |
|
11c |
INSURANCE PLAN NAME OR PROGRAM NAME |
O |
||
11d |
IS THERE ANOTHER HEALTH BENEFIT PLAN? |
S |
Required if applicable. |
|
12 |
PATIENT'S OR AUTHORIZED PERSON'S SIGNATURE |
O |
||
13 |
INSURED'S OR AUTHORIZED PERSONS' SIGNATURE |
N |
||
14 |
DATE OF CURRENT ILLNESS, INJURY OR PREGNANCY (LMP) |
A-7 Date of Injury/Illness |
R |
For Specific Injury: Enter the date [MM DD YYYY] of incident or exposure. Include qualifier 431 for onset of current illness |
15 |
OTHER DATE |
S |
Enter applicable qualifier "454" to denote initial treatment and date [MM DD YYYY] . |
|
16 |
DATES PATIENT UNABLE TO WORK IN CURRENT OCCUPATION |
S |
Required if applicable. Enter the dates [MM DD YYYY] the claimant is unable to work. |
|
17 |
NAME OF REFERRING PROVIDER OR OTHER SOURCE |
S |
Required when Referring Provider [DN], Ordering Provider [DK] or Supervising Provider [DQ] is associated with the bill. Enter applicable qualifier, [DN,DK,DQ], respectively and provider name. |
|
17a |
OTHER ID # |
S |
Enter '0B' qualifier followed by the State License Number of the provider. Required when other provider is associated with the bill. |
|
17b |
NPI # |
S |
Enter NPI of provider in Field 17. Required when other provider is associated with the bill. |
|
18 |
HOSPITALIZATION DATES RELATED TO CURRENT SERVICES |
S |
Required if hospitalization dates [MM DD YYYY] are known. |
|
19 |
ADDITIONAL CLAIM INFORMATION (Designated by NUCC) |
R |
Enter rendering provider information and/or referring, ordering or supervising provider (see item 17). Enter additional identifier (REF) followed by X5 qualifier and WCB Auth# (no spaces). The next data sequence should be separated by 3 spaces followed by the G2 qualifier and the WCB rating code. The next data sequence should be separated by 3 spaces followed by the claim information NTE and the ADD qualifier followed by the name of the rendering provider. |
|
20 |
OUTSIDE LAB? |
S |
Use when billing for diagnostic tests (refer to CMS instructions). |
Top of Section
Item 21 through 33
CMS-1500 Box # |
CMS-1500 (02/12) Field Description |
New York Fields from form C-4 |
New York Workers' Compensation Requirements (Required/ Situational/ Optional / Not Applicable) |
New York Workers' Compensation Instructions |
21 |
ICD IND. |
Blank |
||
21.A |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
D-4 1. ICD 10 |
R |
ICD-10-CM codes are required |
21.B |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
D-4 2. ICD 10 |
S |
ICD-10-CM codes are required, if necessary. |
21.C |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
D-4 3. ICD 10 |
S |
ICD-10-CM codes are required, if necessary. |
21.D |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
D-4 4. ICD 10 |
S |
ICD-10-CM codes are required, if necessary. |
21.E |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
S |
ICD-10-CM codes are required, if necessary. |
|
21.F |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
S |
ICD-10-CM codes are required, if necessary. |
|
21.G |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
S |
ICD-10-CM codes are required, if necessary. |
|
21.H |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
S |
ICD-10-CM codes are required, if necessary. |
|
21.I |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
S |
ICD-10-CM codes are required, if necessary. |
|
21.J |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
S |
ICD-10-CM codes are required, if necessary. |
|
21.K |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
S |
ICD-10-CM codes are required, if necessary. |
|
21.L |
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY Relate Items A-L to service line below (24E) |
S |
ICD-10-CM codes are required, if necessary. |
|
22 |
RESUBMISSION CODE |
O |
||
23 |
PRIOR AUTHORIZATION NUMBER |
S |
Hold for future use by WCB |
|
24A |
DATE(S) OF SERVICE |
D Dates of Service |
R |
First line is required. Subsequent lines are situational |
24B |
PLACE OF SERVICE |
D Place of Service |
R |
First line is required. Subsequent lines are situational |
24C |
EMG |
N |
||
24D |
PROCEDURES, SERVICES, OR SUPPLIES |
D CPT/HCPCS Code |
R |
Enter CPT/HCPCS/DSM-V codes and applicable modifiers. First line is required. Subsequent lines are situational. |
24E |
DIAGNOSIS CODE POINTER |
D Diagnosis Code |
R |
First line is required. Subsequent lines are situational |
24F |
$ CHARGES |
D Charges |
R |
First line is required. Subsequent lines are situational |
24G |
DAYS OR UNITS |
D Days or Units |
R |
Enter number of days or units. If reporting a fraction of a unit, use the decimal point. First line is required. Subsequent lines are situational |
24H |
EPSDT/FAMILY PLAN |
N |
||
24I Grey |
ID QUAL |
R |
Required. Use qualifier "0B" for State License Number. First line required. Subsequent lines are situational. |
|
24J Grey |
RENDERING PROVIDER ID. # |
R |
Report State License Number. First line required. Subsequent lines are situational. |
|
24J |
NPI# |
C-10 Tx Provider NPI # |
R |
NPI# required, if available. First line required. Subsequent lines are situational. |
24 Grey |
GREY AREA SUPPLEMENTAL DATA |
|||
25 |
FEDERAL TAX ID. NUMBER |
C-4 Fed Tax ID # SSN or EIN? |
R |
|
26 |
PATIENT'S ACCOUNT NO. |
A-12 Patient Account # |
R |
|
27 |
ACCEPT ASSIGNMENT? |
R |
Yes is required. No is Not applicable. |
|
28 |
TOTAL CHARGE |
D Total Charge |
R |
|
29 |
AMOUNT PAID |
D Amount Paid |
S |
|
30 |
RSVD FOR NUCC USE |
N |
||
31 |
SIGNATURE OF PHYSICIAN OR SUPPLIER |
R |
||
32 |
SERVICE FACILITY LOCATION INFORMATION |
R |
Name, Address, City, State and Zipcode of service location |
|
32a |
NPI # |
S |
Required if NPI# is known |
|
32b |
OTHER ID # |
S |
Enter state license number if service facility location is not eligible for an NPI. |
|
33 |
BILLING PROVIDER INFO & PH # |
C-1 Last Name, First Name, MI |
R |
Required as provided in 1500 Health Insurance Claim Form Reference Manual |
33a |
NPI # |
S |
Required if NPI# is known |
|
33b |
OTHER ID # |
S |
Enter state license number if billing provider location is not eligible for an NPI. |
Top of Section
Back to Top
Additional Resources
New York State Workers' Compensation Board CMS-1500 Initiative
daisyBill Solution
Stay up-to-date on the latest developments in Workers’ Compensation medical billing by subscribing to daisyBill’s email list.